Many older adults take five, six, or even more medications every day. Some of these pills were prescribed years ago for conditions that have changed-or even disappeared. But no one ever asked if they still needed them. You might feel tired all the time, dizzy when you stand up, or confused after taking your evening pills. You think, Is this normal at my age? The truth? It’s not. And you don’t have to live with it.
Why Talking About Reducing Medications Matters
Taking too many drugs isn’t just inconvenient-it’s dangerous. About 15% of seniors on five or more medications experience harmful side effects like falls, memory problems, or kidney damage. These aren’t rare events. They happen every day. And the worst part? Many of these drugs no longer help. They’re just adding risk. Deprescribing isn’t about stopping everything. It’s about removing what’s no longer useful. It’s about keeping only what improves your life. The goal isn’t fewer pills-it’s better days. You want to walk your dog without feeling shaky. You want to sleep through the night. You want to remember your grandchild’s name without struggling.What Deprescribing Really Means
Deprescribing means slowly and safely reducing or stopping medications when the risks outweigh the benefits. It’s not withdrawal. It’s optimization. Think of it like cleaning out your closet-you keep what fits, what you wear, what makes you feel good. Everything else? It’s just taking up space. Doctors don’t always bring this up. A 2023 study found that 68% of seniors would like to take fewer medications, but only 12% ever had the conversation. Why? Because patients wait for the doctor to start it. And too often, they don’t. The good news? You don’t need to wait. You can lead this conversation. And when you do, success rates jump by 92%.How to Prepare Before Your Appointment
Walking into a doctor’s office and saying, “I want to take fewer pills” rarely works. It sounds vague. It feels like you’re arguing against medicine itself. Instead, prepare like you’re getting ready for a job interview. Here’s what works:- Write down every medication-prescription, over-the-counter, vitamins, supplements. Don’t forget the aspirin you take for heart health or the melatonin you use for sleep. Many patients leave out OTC drugs, and those are often the ones causing trouble.
- Track side effects. Not just “I feel tired.” Write: “Dizziness 2 hours after taking metoprolol, almost fell on Tuesday and Friday last week.” Specifics matter. Doctors notice patterns.
- Choose 1 or 2 meds to focus on. Don’t try to tackle all of them at once. Pick the one causing the most trouble-the one making you feel worse than the condition it treats.
- Write down your goal. Not “I want fewer pills.” Say: “I want to stop feeling so dizzy so I can garden again.” Or: “I want to sleep through the night without taking three different pills.” Goals connect medicine to your life.
Patients who do this are 37% more likely to have a successful deprescribing plan. Why? Because you’re not asking for a favor-you’re offering a clear path forward.
How to Start the Conversation
The best way to begin isn’t with a demand. It’s with a question. Try this:- Ask: “What’s your view on how my medications are working for me right now?”
- Tell: “I’ve been feeling dizzy after my morning dose of amlodipine. I’ve also noticed I’m forgetting things more often. I’m worried these meds might be doing more harm than good.”
- Ask again: “What would be the safest way to test if we could reduce one of these?”
This is called the “ask-tell-ask” method. It’s used by top geriatricians because it turns a lecture into a conversation. You’re not challenging your doctor-you’re inviting them to help you solve a problem.
Studies show this approach increases successful deprescribing by 58% compared to just asking for pills to be cut.
What to Say When They Push Back
Your doctor might say:- “This medicine is for your blood pressure.”
- “You’ve been on this for years.”
- “What if you have a heart attack?”
Don’t get defensive. Respond with facts and feelings.
Try this:
- “I understand it was helpful before. But my blood pressure is now 110/70-consistently. I’m on three blood pressure pills. Is it possible one is enough now?”
- “I’ve read that some medications become riskier as we age, especially for memory and balance. I’m not asking to stop everything-just to check if one could be reduced safely.”
- “My goal is to stay independent. If I keep falling, I won’t be able to live alone. I’d rather avoid that risk.”
People respond better to stories than statistics. Saying, “I want to walk my granddaughter to school without feeling dizzy” is 4.7 times more effective than saying, “This drug causes dizziness.”
What Medications Are Most Often Safe to Reduce?
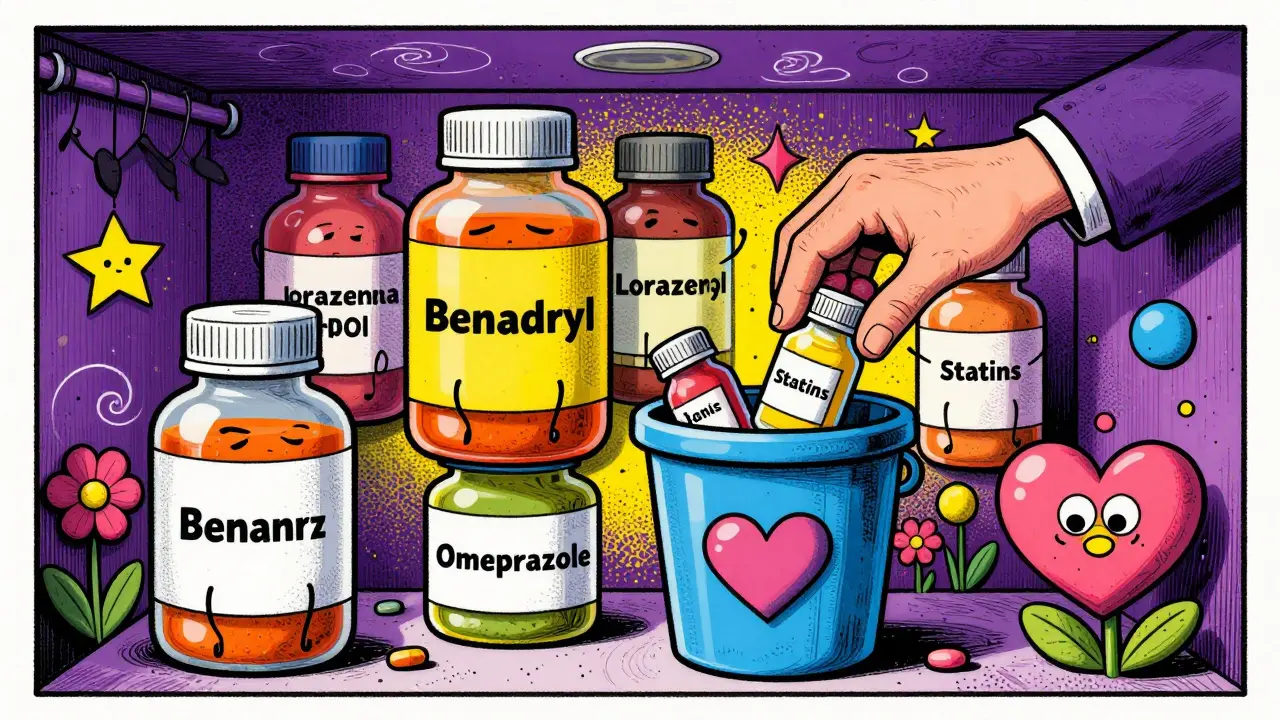
Not all meds are equal. Some are more likely to cause harm than help in older adults. Here are the top five categories doctors commonly consider for deprescribing:- Anticholinergics (like diphenhydramine/Benadryl, oxybutynin) - linked to confusion and memory loss.
- Benzodiazepines (like lorazepam, alprazolam) - increase fall risk and dementia risk over time.
- Proton pump inhibitors (like omeprazole) - often used long-term for heartburn, but can cause nutrient loss and infections.
- Statins - for some seniors over 75 without heart disease, the benefit is small and side effects (muscle pain, fatigue) are common.
- Multiple blood pressure meds - especially if your numbers are consistently low (under 120/70).
You don’t need to know all this. But if you’ve heard of the Beers Criteria or STOPP/START guidelines, bring a printed summary. Patients who do are 33% more likely to have their concerns taken seriously.
Expect Gradual Changes-Not Quick Fixes
No one should stop a medication cold turkey. That’s dangerous. Most successful deprescribing happens slowly. Ask for a plan:- “Could we lower my dose by 25% every month and check in after each change?”
- “Can we do a ‘drug holiday’-stop it for two weeks and see how I feel?”
- “What symptoms should I watch for if we reduce this?”
Eighty-six percent of successful deprescribing cases use gradual steps. Your doctor will want to monitor you. That’s normal. Bring a notebook to track how you feel each week. Note sleep, energy, balance, mood.

What If They Say No?
Sometimes, doctors say no. Maybe they’re pressed for time. Maybe they’re unsure. Maybe they’re worried about liability. Don’t give up. Say: “I understand you’re not ready to change this now. Could we schedule a follow-up in 3 months to check how I’m doing? I’d like to see if I feel better with fewer meds.”Most doctors will agree to a follow-up. And if you come back with notes showing improvement-like fewer falls, better sleep, or more energy-they’ll be more likely to act next time.
It’s Not Just About Pills-It’s About Your Life
Medications aren’t the enemy. But when they start stealing your independence, your peace, your joy-they become part of the problem. You’re not being difficult. You’re being smart. You’re using your own experience to guide your care. And that’s exactly what good medicine should be.More seniors are starting these conversations now. Medicare now requires medication reviews during annual wellness visits. Electronic systems flag risky meds. Public awareness campaigns are growing. You’re not alone.
Take your list. Write your goal. Ask the right questions. And don’t let anyone tell you that taking fewer pills means giving up on your health. Sometimes, it’s the most powerful thing you can do to protect it.
Is deprescribing the same as stopping all my medications?
No. Deprescribing means carefully removing medications that no longer help-or that cause more harm than benefit. It’s not about stopping everything. It’s about keeping only what improves your daily life, like your energy, balance, or sleep. Many people end up with fewer pills, but the ones they keep work better for them.
What if I’m afraid my condition will get worse if I stop a medication?
That fear is common-and valid. That’s why deprescribing is always done slowly and with monitoring. Your doctor will suggest a taper, not an abrupt stop. You’ll track symptoms like blood pressure, mood, or dizziness. If something changes, you can restart the medication. Most people find their condition stays stable or even improves once unnecessary drugs are removed.
Can I just stop a medication on my own if I think it’s not helping?
No. Some medications, like blood pressure pills, antidepressants, or steroids, can cause serious withdrawal effects if stopped suddenly. Even if you feel fine, stopping without medical guidance can be dangerous. Always work with your doctor to create a safe plan. They know how to adjust doses gradually to avoid rebound effects.
How do I know which medications are safe to reduce?
There are evidence-based lists like the Beers Criteria and STOPP/START guidelines that identify medications often risky for older adults. These include things like long-term proton pump inhibitors, anticholinergics (like Benadryl), and multiple blood pressure drugs. You don’t need to memorize them-just bring your full list to your doctor and ask, “Are any of these on the list of medications that can be risky for seniors?”
What if my doctor says I need all these meds for my health?
Ask for specifics. Say: “Can you explain how each one is helping me right now? What’s the goal for this medication?” If they can’t say, it’s a red flag. Also ask: “If I were to stop this one, what would you watch for?” If they’re willing to monitor you, that’s a good sign. If they dismiss your concerns without explanation, consider asking for a referral to a geriatrician or pharmacist who specializes in senior medications.
Will my insurance or Medicare cover a medication review?
Yes. Since 2024, Medicare requires an annual medication review as part of the Annual Wellness Visit. You don’t need to pay extra. Just ask your doctor to include a “medication optimization discussion” when you schedule your appointment. Many primary care offices now bill for this service, so it’s in their interest to make time for it.
Can I bring someone with me to the appointment?
Absolutely. In fact, it’s encouraged. A family member or caregiver can help remember details, ask questions you might forget, and support you if you feel overwhelmed. Many doctors welcome a second set of ears-especially when discussing complex medication changes. Just let the office know ahead of time so they can make space.
Next Steps: What to Do Right Now
1. Write down every pill, patch, and supplement you take-even the ones you only take “as needed.”You’ve spent years taking care of others. Now it’s time to take care of yourself-by making sure your medications serve you, not the other way around.








January 2, 2026 AT 09:46
Kristen Russell
Finally, someone said it out loud. I’ve been telling my dad for years to ask his doctor about cutting his meds-he’s on 8 pills and can barely walk without dizziness. He just thought it was ‘getting old.’ Not anymore.
January 3, 2026 AT 11:25
Lee M
Deprescribing isn’t weakness-it’s intellectual courage. The medical-industrial complex thrives on perpetual prescription cycles. We’ve turned aging into a pathology to be managed, not a stage of life to be lived. You don’t need more drugs-you need more clarity.
January 5, 2026 AT 07:29
Bryan Anderson
This is such an important topic. I’ve seen elderly patients in my practice who’ve been on the same statin for 15 years with no documented cardiovascular risk. The inertia in prescribing is real. Thank you for outlining practical steps-it’s exactly what’s missing in most conversations.
January 5, 2026 AT 09:27
Matthew Hekmatniaz
I grew up in a culture where elders were rarely questioned. But here, in the U.S., I’ve seen how overmedication robs dignity. My aunt stopped her anticholinergic after reading this-and she started recognizing people again. Small changes, huge impact.
January 5, 2026 AT 10:06
Liam George
They don’t want you to reduce meds because Big Pharma owns the FDA, the AMA, and your doctor’s continuing education. They’re selling dependency. The ‘Beers Criteria’? A loophole. The real agenda? Keep you docile, keep you paying, keep you hooked. Wake up.
January 7, 2026 AT 02:34
sharad vyas
In India, we say: ‘Too many medicines, too little peace.’ This article is true. My grandfather took three pills for blood pressure. One was enough. He lived to 92, walked daily, remembered everyone’s name. Simple life, simple care.
January 8, 2026 AT 03:11
Dusty Weeks
bro this is lit 🙌 i was just telling my grandma last week to stop taking that benadryl for sleep 😭 she said ‘but it’s over the counter!’ nooo that’s the worst part!!!
January 9, 2026 AT 00:38
Sally Denham-Vaughan
My mom did this last year-cut her PPI and her acid reflux got better. She’s sleeping through the night and actually eating dinner without a nap after. I wish I’d pushed harder sooner. Thanks for the nudge.
January 10, 2026 AT 03:50
Bill Medley
The clinical evidence supporting deprescribing in geriatric populations is robust and well-documented. The reluctance among primary care providers stems from systemic time constraints and liability concerns, not clinical uncertainty.
January 11, 2026 AT 02:26
Richard Thomas
It’s fascinating how medicine has become a transactional enterprise rather than a relational one. We’ve lost the art of listening-of observing how a patient moves, how they speak, how they carry themselves-instead of just checking boxes on a form. Deprescribing isn’t just about pills; it’s about returning agency to the person who’s lived with their body longer than any clinician ever has. It’s about dignity. It’s about presence. It’s about recognizing that sometimes, the most therapeutic intervention is silence, followed by a thoughtful question: ‘What do you want your days to feel like?’
January 11, 2026 AT 18:54
Paul Ong
Write down your meds. Write down your goal. Call the office. That’s it. No fancy jargon. No drama. Just do it. Your life is worth it
January 12, 2026 AT 11:00
Andy Heinlein
my uncle just stopped his benzos last month and now he’s playing guitar again 😭 he said he forgot what it felt like to be awake. this post saved him
January 13, 2026 AT 06:33
Ann Romine
I brought my mom’s full med list to her appointment and asked if any were on the Beers Criteria. The doctor paused, looked at me, and said, ‘You’re the first family member who’s ever done this.’ We cut two meds. She’s been sleeping better since.
January 13, 2026 AT 08:37
Todd Nickel
The psychological barriers to deprescribing are profound. Patients often conflate medication with care-ceasing a drug feels like abandonment, even when it’s medically appropriate. Providers, meanwhile, fear malpractice and default to continuation bias. The solution lies not in more guidelines, but in structural incentives: reimbursement for medication reconciliation, mandatory geriatric training, and standardized decision aids embedded in EHRs. Until then, empowered patients remain the most effective catalyst for change.
January 13, 2026 AT 19:50
Austin Mac-Anabraba
Let’s be honest: 90% of these ‘medication reviews’ are performative. Doctors know the risks, but they’re too lazy to adjust. They’ll nod along, then refill everything next month. The system is designed to keep you medicated, not healed. This article is a Band-Aid on a hemorrhage.