Why Heat Turns Common Medications Into Hidden Dangers for Seniors
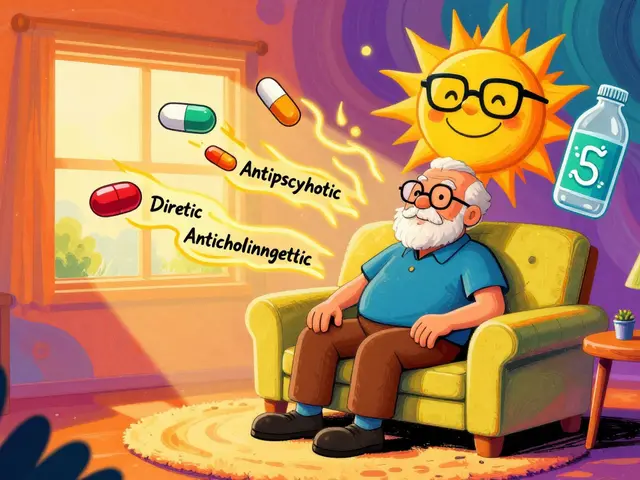
When the temperature rises, most people think about drinking more water or turning on the AC. But for seniors on certain medications, heat isn’t just uncomfortable-it’s life-threatening. The body’s ability to cool down weakens with age, and many everyday prescriptions make that problem worse. A 78-year-old taking a diuretic for high blood pressure might not feel thirsty, even as their body loses fluids. Someone on an antipsychotic for dementia might not sweat at all, letting their core temperature climb silently. These aren’t rare cases. Heat-related medication problems are one of the fastest-growing health risks for older adults, especially as summers get hotter and longer.
The CDC reports that heat-related deaths among seniors have jumped 67% since 2004. And it’s not just about the weather-it’s about what’s in the medicine cabinet. About 87% of adults over 65 take two or more prescription drugs. Many of those drugs interfere with how the body handles heat. That’s why simply telling seniors to "stay hydrated" isn’t enough. You need to know which medications are dangerous in the heat, what to watch for, and how to act before it’s too late.
Medications That Turn Up the Heat Risk
Not all drugs are equal when it comes to heat. Some are quietly sabotaging the body’s natural cooling system. Here are the top offenders:
- Diuretics (like hydrochlorothiazide, furosemide): These are called "water pills" because they help the body get rid of extra fluid. But they also reduce thirst by 30-40%, so seniors don’t drink enough-even when they should. They also flush out sodium and potassium, leading to dangerous electrolyte imbalances. A sodium level below 135 mmol/L is a red flag.
- ACE inhibitors and ARBs (like benazepril, losartan): These blood pressure meds lower thirst by about 25%. They also reduce blood volume, making it harder for the body to circulate blood to the skin to cool down.
- Antipsychotics (like quetiapine, clozapine): Used for dementia or schizophrenia, these drugs disrupt the brain’s thermostat. Studies show they can raise core body temperature by 1.5-2.0°F even without physical activity.
- Anticholinergics (like diphenhydramine in Benadryl or Tylenol PM): These block sweat glands. Seniors on these meds may sweat 35-50% less, making heat dissipation nearly impossible.
- Some antibiotics and antifungals: Drugs like doxycycline or griseofulvin make skin ultra-sensitive to sunlight. Sunburn can happen in half the time, and severe burns can trigger heat stress.
The worst part? These risks multiply when meds are combined. A senior on a diuretic plus an ACE inhibitor is at double the risk. Their blood volume drops, they don’t feel thirsty, and their body can’t sweat. That’s a recipe for heat stroke.
What to Do Before Summer Hits
Waiting until it’s 90°F outside to think about meds is too late. Prevention starts months before the heat arrives.
First, get a full medication review with a pharmacist or doctor. Don’t just talk about side effects-ask: "Which of these drugs make me more vulnerable to heat?" Write down every pill, supplement, and over-the-counter drug. Include things like sleep aids, allergy meds, and pain relievers. Many seniors don’t realize Tylenol PM or Benadryl are risky.
Next, ask about adjustments. Can your diuretic dose be lowered on hot days? Can you switch from a long-acting anticholinergic to a safer alternative? The CDC says medication changes during heat waves can reduce emergency visits by up to 37%. But you need to plan this ahead of time-not in the middle of a heat emergency.
Also, check fluid restrictions. Many seniors with heart failure are told to limit water. But during heat waves, those restrictions can become deadly. Talk to your doctor about temporary, safe increases in fluid intake. Don’t guess-get clear instructions.
Hydration That Actually Works
Drinking water isn’t optional-it’s non-negotiable. But it’s not as simple as "drink eight glasses a day."
- Drink water every hour, even if you’re not thirsty. Thirst is already a late signal in seniors.
- Avoid caffeine and alcohol. Both act as diuretics and can make dehydration worse by increasing urine output by 40-60%.
- If you’re on a diuretic, choose electrolyte drinks with 120-150 mg of sodium per 8 oz. Plain water alone won’t replace what you’re losing.
- Coconut water, broth, or oral rehydration solutions (like Pedialyte) are better than sports drinks, which often have too much sugar.
- Keep water within reach at all times-bedside, chair, car. Use a marked bottle to track intake.
For seniors with swallowing issues or memory problems, caregivers should offer fluids on a schedule-not just when asked. A simple hourly reminder can save a life.
Environment Matters More Than You Think
Staying cool isn’t just about the thermostat-it’s about your whole environment.
- Keep indoor temps below 78°F (25.6°C). If you don’t have AC, find a cool public space-libraries, malls, community centers. Many offer free cooling centers during heat waves.
- Use fans only if the air is cooler than body temperature. In extreme heat, fans can blow hot air around and make things worse.
- Wear loose, light-colored cotton clothes. Synthetic fabrics trap heat. Cotton can lower perceived temperature by 5-7°F.
- Use broad-spectrum SPF 15+ sunscreen and reapply every two hours-or after sweating. Some meds make sunburn happen 4-6 times faster.
- Stay indoors between 10 a.m. and 4 p.m., when temperatures peak. Plan errands for early morning or evening.
Assisted living facilities that use the "I’m OK" check-in system-where staff monitor temperature and mental state daily-have cut heat-related hospitalizations by 33%. Simple routines make a huge difference.
Recognizing the Warning Signs (Before It’s Too Late)
Heat exhaustion and heat stroke don’t always look like what you see in movies. Seniors often show subtle, confusing signs.
Heat exhaustion symptoms:
- Heavy sweating (but sometimes none at all, if on anticholinergics)
- Muscle cramps
- Headache, nausea, vomiting
- Dizziness, weakness, fatigue
- Fainting or feeling lightheaded
Here’s the scary part: 41% of seniors don’t show classic symptoms. Instead, they become confused, agitated, or unusually quiet. That’s not just "getting old"-it’s a sign their brain is overheating.
Heat stroke is a medical emergency:
- Body temperature above 103°F (39.4°C)
- Hot, dry, or damp skin (no sweating)
- Rapid, strong pulse
- Confusion, slurred speech, unconsciousness
If you see any of these, call 911 immediately. Don’t wait. The CDC says 65% of heat exhaustion cases turn into heat stroke within 2-4 hours if untreated.
What to Do Right Away
If you suspect heat stress, act fast:
- Move the person to a cool, shaded, or air-conditioned place.
- Remove excess clothing.
- Apply cool, wet cloths to the skin-or give a cool shower or sponge bath.
- Give small sips of cool water or electrolyte drink-if they’re alert and able to swallow.
- Do NOT give alcohol, caffeine, or sugary drinks.
- Call 911 if symptoms don’t improve in 30 minutes, or if they’re confused, unconscious, or have a high fever.
Never assume someone is "just tired" or "acting strange." In seniors on risky meds, those are early warning signs.
New Tools to Help You Stay Safe
There’s new tech making prevention easier.
The CDC’s Heat and Medication Risk Assessment Tool (HM-RAT), launched in 2023, lets you input a senior’s meds and get a personalized heat risk score. It even factors in local weather forecasts.
HeatRisk.gov, a joint project of the National Institute on Aging and the EPA, gives daily heat alerts tailored to medication users. Over 1.2 million seniors used it during the 2023 summer season.
And research is underway for a new "heat resilience" supplement designed for seniors on multiple meds. Early trials show it improves thermoregulation by 28%. While not yet available, it shows how seriously this problem is being taken.
Final Thought: This Isn’t Just About Comfort-It’s About Survival
By 2050, extreme heat days could increase by 50%. That means more seniors will be at risk. The good news? Almost all heat-related deaths in this group are preventable. It doesn’t take fancy equipment or expensive solutions. It takes awareness, planning, and action.
Start today. Look at the medication list. Talk to the doctor. Set up a hydration schedule. Check the weather forecast. Make a plan. You’re not just helping someone stay cool-you’re helping them stay alive.
Can seniors stop taking their meds during a heat wave?
No. Never stop or change medication without talking to a doctor. Stopping blood pressure or heart meds suddenly can cause stroke, heart attack, or dangerous rebound effects. Instead, ask your provider if the dose can be temporarily adjusted or if a safer alternative exists during hot weather.
What’s the safest way to cool down a senior during a heat emergency?
Move them to a cool place immediately. Use wet cloths on the neck, armpits, and groin-areas where blood vessels are close to the skin. A cool shower or sponge bath works well. Avoid ice baths, which can cause shock. Fan them gently while keeping them lying down. Call 911 if they’re confused, unconscious, or have a fever above 103°F.
Are over-the-counter meds like Benadryl safe in summer?
No. Benadryl (diphenhydramine) and similar antihistamines block sweating and can raise body temperature. Many seniors take them for sleep or allergies, not realizing the danger. Switch to non-anticholinergic options like loratadine (Claritin) or cetirizine (Zyrtec) for allergies, and melatonin or behavioral sleep strategies instead of sleep aids.
How often should seniors have their meds reviewed for heat risks?
At least once a year, and always before summer. But if they’ve started a new medication, changed doses, or had a hospital stay, get a review right away. The American Geriatrics Society recommends a formal medication review every 6-12 months for seniors on three or more drugs.
Is air conditioning necessary, or are fans enough?
Fans alone aren’t enough when temperatures exceed 90°F. In extreme heat, fans just circulate hot air and can make things worse. Air conditioning is the safest option. If you can’t afford AC, go to public cooling centers-libraries, community centers, and malls often open them during heat warnings. Never rely on a fan alone for seniors on heat-risk meds.




January 26, 2026 AT 21:05
Candice Hartley
This is so important 😭 My grandma was on diuretics and didn't realize she was dehydrating until she passed out. I wish this was in every doctor's office.
January 28, 2026 AT 04:58
Kathy McDaniel
i had no idea benadryl was this dangerous in heat 😳 my mom takes it every night for sleep... gotta talk to her dr ASAP
January 29, 2026 AT 04:50
Desaundrea Morton-Pusey
another liberal scare tactic. people have been taking meds for decades and we're fine. just stop whining about the weather.
January 30, 2026 AT 07:10
John O'Brien
bro this is legit life or death. i work in home care and saw a guy go into heat stroke because he was on quetiapine and thought he was just 'tired'. he ended up in the ICU for two weeks. don't sleep on this.
January 30, 2026 AT 17:24
Kegan Powell
we think of heat as just uncomfortable but its actually a silent killer for so many seniors on meds... its like the body is slowly being betrayed by the very things meant to help it. we need to treat this like a public health emergency not just a summer tip
January 31, 2026 AT 18:07
April Williams
if your parent is on these meds and you're not monitoring them 24/7 you're neglecting them. why are people still letting their elderly relatives live alone? this is preventable if you just care enough to check in
February 1, 2026 AT 16:11
Andrew Clausen
The CDC's 67% increase statistic is misleading. It does not account for improved reporting, aging population demographics, or increased diagnostic criteria. Correlation does not equal causation.
February 3, 2026 AT 01:38
Anjula Jyala
Anticholinergic burden is the real issue here. Polypharmacy in elderly population leads to cholinergic deficit which impairs thermoregulatory中枢. You must stratify by Beers Criteria and deprescribe where possible
February 4, 2026 AT 12:06
Kirstin Santiago
I've seen this firsthand with my aunt. She was on a diuretic and an ACE inhibitor and didn't drink water because she didn't feel thirsty. We started setting alarms every hour for her to sip water and it made all the difference. You don't need to be a doctor to save a life here.
February 4, 2026 AT 18:20
Paul Taylor
you know what really gets me is how nobody talks about the fact that most seniors on these meds are also on multiple other drugs and the interactions are a nightmare. i mean like one guy i knew was on a diuretic plus an anticholinergic plus an antibiotic plus a sleep aid and he thought he was fine because he didn't have a fever but his body was shutting down from the inside out and no one caught it until he collapsed in the grocery store and by then it was too late and that was the last time i ever took anything for granted about my parents health
February 5, 2026 AT 02:46
Murphy Game
this is all a government ploy to get seniors to buy AC units. they know the power companies are making bank in summer. and that HM-RAT tool? it's tracking your meds and selling data to Big Pharma. don't fall for it.