Carbamazepine Drug Interaction Calculator
How Carbamazepine Affects Your Medications
Carbamazepine is a strong CYP3A4 inducer that can reduce levels of many medications by 30-80%. Enter your medication below to see how it might be affected and what dose adjustments may be needed.
Carbamazepine isn't just another seizure medication. If you're taking it, or prescribing it, you need to understand one hard truth: carbamazepine changes how your body handles almost every other drug you're on. It doesn't just sit there-it actively rewires your liver's ability to break down medications. And that can be dangerous if you don't know what you're dealing with.
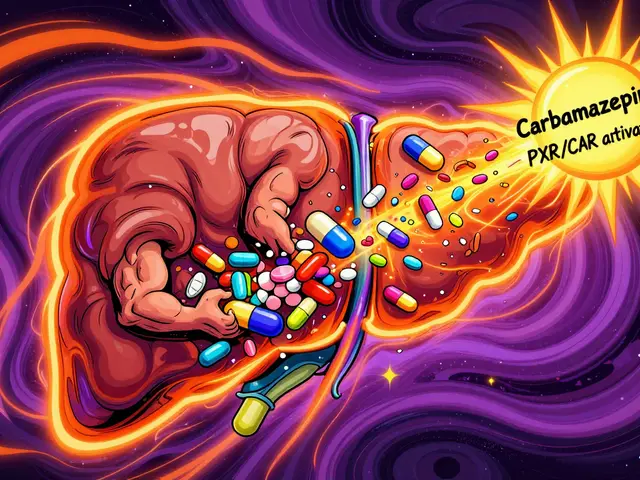
How Carbamazepine Turns Your Liver Into a Drug-Cleaning Machine
Carbamazepine doesn't work by blocking receptors or calming nerves directly. Instead, it flips a switch in your liver cells. It activates two nuclear receptors-PXR and CAR-that tell your body to make more of certain enzymes, especially CYP3A4 and CYP2B6. These enzymes are the main workers in your liver that break down drugs. When carbamazepine turns them up, your body starts chewing through other medications faster than normal.
This isn't a minor effect. Carbamazepine is classified by the FDA as a strong CYP3A4 inducer. That puts it in the same league as rifampicin, one of the most powerful enzyme inducers known. Studies show it can slash the blood levels of drugs metabolized by CYP3A4 by 60 to 80%. For example, when taken with simvastatin (a cholesterol drug), carbamazepine reduces its concentration by 74%. That means the statin barely works anymore.
What makes this even trickier is that carbamazepine does this to itself. This is called autoinduction. When you start taking carbamazepine, your body slowly ramps up its own metabolism. Within 3 to 4 weeks, your plasma levels drop by 30 to 50%. That’s why doctors often start patients on low doses and gradually increase them. If you don’t adjust the dose, you risk breakthrough seizures because the drug isn’t staying in your system long enough.
The Drugs That Get Washed Out by Carbamazepine
Carbamazepine doesn’t pick and choose. It affects a wide range of medications across multiple classes. Here’s what you need to watch for:
- Oral contraceptives: Ethinyl estradiol levels can drop by 50 to 70%. There are documented cases of unintended pregnancies in women taking both carbamazepine and birth control pills. Even if you’ve been on the pill for years, adding carbamazepine can make it useless.
- Anticoagulants like warfarin: Carbamazepine speeds up warfarin breakdown, lowering INR levels. Patients often need to increase their warfarin dose by 50 to 100% to stay in the therapeutic range. Without monitoring, this can lead to dangerous clots.
- Antidepressants: SSRIs like sertraline, SNRIs like venlafaxine, and tricyclics like amitriptyline all get metabolized faster. This can lead to treatment failure-patients feel like the antidepressant stopped working, when in reality, their body is clearing it too fast.
- Immunosuppressants: Cyclosporine, tacrolimus, and sirolimus levels can plummet. Transplant patients on carbamazepine have had organ rejection because their immune-suppressing drugs were no longer effective.
- Benzodiazepines: Alprazolam, diazepam, and clonazepam lose potency. Patients may feel anxious or have trouble sleeping even though they’re taking the same dose.
- Statins: Simvastatin and lovastatin become ineffective. Atorvastatin is less affected, but still needs monitoring.
- HIV and hepatitis C drugs: Protease inhibitors and direct-acting antivirals like elbasvir/grazoprevir are severely impacted. This can lead to treatment failure and drug resistance.
A 2017 study of over 2,400 patients on carbamazepine found that nearly 4 out of 10 needed dose changes because of interactions. The biggest culprits? Anticoagulants, antidepressants, and immunosuppressants.

Why This Isn’t Just About Dosing-It’s About Timing
Many clinicians miss the timing part. Carbamazepine doesn’t induce enzymes overnight. It takes about 14 days to reach full effect. That’s why you can’t just check a drug interaction app and assume you’re safe. A patient might start carbamazepine and then get prescribed a new medication a week later. Everything looks fine at first. Then, two weeks later, the new drug stops working. That’s when the real problem shows up.
And it works both ways. When you stop carbamazepine, the enzyme levels don’t drop immediately. It can take weeks for CYP3A4 activity to return to normal. So if you discontinue carbamazepine and leave other drugs at the same dose, those drugs can suddenly build up to toxic levels. There are case reports of patients developing severe sedation or respiratory depression after stopping carbamazepine while still taking alprazolam. The body wasn’t ready to slow down drug clearance.
How to Manage These Interactions in Real Life
There’s no magic fix. But there are proven steps to stay safe:
- Check everything before you start: Review every medication the patient is taking-prescription, OTC, even herbal supplements. St. John’s wort? It’s also a CYP3A4 inducer. Combine it with carbamazepine and you’re stacking the deck.
- Monitor drug levels: Therapeutic drug monitoring isn’t optional. Check carbamazepine levels at baseline, then at 2 and 4 weeks after starting or changing the dose. Also monitor levels of interacting drugs like warfarin (INR), cyclosporine, and antidepressants if possible.
- Adjust doses before and after: When adding carbamazepine, anticipate needing higher doses of other drugs. When stopping it, plan to reduce those other drugs by 25 to 50% over 2 to 4 weeks.
- Use alternatives when possible: For epilepsy, eslicarbazepine is a newer option with 80% less enzyme induction. For bipolar disorder, lamotrigine or valproate may be safer choices if interactions are a concern.
- Use tools: The Open Systems Pharmacology model from Fuhr et al. (2021) is a free, publicly available tool for predicting these interactions. It’s not plug-and-play, but with 8 to 16 hours of training, pharmacists can use it to model real-world scenarios.
The American Academy of Neurology recommends baseline and follow-up TDM for all patients starting carbamazepine. It’s not just good practice-it’s necessary.
What’s Changing in the Field
Carbamazepine isn’t disappearing. In 2022, there were over 4.2 million prescriptions in the U.S. It’s still a go-to for focal seizures and trigeminal neuralgia. But its role is shrinking. Newer drugs like lacosamide and cenobamate don’t induce enzymes, and they’re gaining ground.
The 2023 FDA approval of extended-release carbamazepine-ASP (Apitegromab) was a step forward. It delivers more stable blood levels, which reduces the peak-and-trough swings that drive autoinduction. Early data suggests it lowers interaction potential by about 30%.
And research is moving toward personalized dosing. Scientists are studying genetic variants in PXR and CAR receptors to predict who will be a strong inducer and who won’t. A clinical trial (NCT05678901) is currently underway at the NIH to see if genetic testing can guide carbamazepine dosing to minimize interactions.
Still, for now, carbamazepine remains one of the most clinically significant enzyme inducers we have. It’s not the easiest drug to manage, but it’s still essential for many patients. The key isn’t avoiding it-it’s knowing how to use it without putting patients at risk.
What Happens When You Don’t Pay Attention
Real-world stories tell the real story. A 32-year-old woman on carbamazepine for seizures got pregnant after being on birth control for five years. Her OB-GYN blamed her. The pharmacist later found the interaction. A man on warfarin for a mechanical heart valve had a stroke after his carbamazepine dose was increased. His INR had dropped from 2.8 to 1.4. A bipolar patient on lamotrigine had a seizure after starting carbamazepine-his lamotrigine levels had crashed by 60%.
These aren’t rare cases. They’re predictable. And they’re preventable.
Does carbamazepine affect all medications the same way?
No. Carbamazepine mainly affects drugs metabolized by CYP3A4, CYP2B6, CYP2C9, CYP2C19, and UGT enzymes. Medications that are excreted unchanged in the urine or metabolized by other pathways (like CYP2D6) are less affected. For example, fluoxetine and paroxetine are mostly metabolized by CYP2D6, so they’re less likely to interact. But drugs like simvastatin, cyclosporine, and oral contraceptives are highly vulnerable.
How long does it take for carbamazepine to start inducing enzymes?
It takes about 10 to 14 days to reach full enzyme induction. Some markers, like the urinary 6β-hydroxycortisol/cortisol ratio, plateau around 60 hours after starting, but full induction of CYP3A4 takes longer. That’s why interactions often show up weeks after starting carbamazepine-not immediately.
Can I just increase the dose of the other drug to fix the interaction?
Sometimes, but it’s risky. Increasing doses without monitoring can lead to toxicity if carbamazepine is later stopped. For example, raising the dose of alprazolam to counteract carbamazepine’s effect could cause severe sedation or respiratory depression once carbamazepine is discontinued. Always plan for both the start and stop of carbamazepine.
Is therapeutic drug monitoring really necessary?
Yes. Carbamazepine has a narrow therapeutic range (4-12 µg/mL), and autoinduction causes levels to drop unpredictably. Without monitoring, patients can have breakthrough seizures or toxicity. For interacting drugs like warfarin or cyclosporine, regular lab checks are essential. The American Academy of Neurology recommends baseline, 2-week, and 4-week monitoring after starting or changing the dose.
Are there safer alternatives to carbamazepine?
Yes. For epilepsy, drugs like lacosamide, levetiracetam, and cenobamate have minimal enzyme induction. For bipolar disorder, lamotrigine and valproate are often preferred. Eslicarbazepine, a newer analog of carbamazepine, causes 80% less CYP3A4 induction and is now approved in the U.S. and EU. These alternatives reduce interaction risks significantly.
What should I do if I’m prescribed carbamazepine and already take other meds?
Don’t stop anything. Talk to your pharmacist or prescriber immediately. Bring a complete list of all medications, including supplements and over-the-counter drugs. Ask specifically: "Will carbamazepine affect how my other drugs work?" Request therapeutic drug monitoring for both carbamazepine and any interacting drugs. Plan for dose adjustments both when starting and stopping carbamazepine.







January 22, 2026 AT 07:11
Chiraghuddin Qureshi
Bro this is wild 😱 I’m in India and my cousin’s neurologist just switched him from phenytoin to carbamazepine - told him to watch out for his birth control. He laughed until his girlfriend got pregnant. Now he’s got a baby and a new pharmacy bill. 🤯
January 22, 2026 AT 11:49
Oren Prettyman
While I appreciate the clinical detail presented herein, I must express my profound concern regarding the lack of citation for the 2021 Open Systems Pharmacology model referenced in the fifth management recommendation. The absence of a DOI, author affiliation, or peer-reviewed publication status renders this assertion speculative at best and potentially misleading to non-specialist readers who may place undue trust in unverified computational models. Furthermore, the assertion that eslicarbazepine reduces induction by 80% is overstated; the original 2018 meta-analysis by Kwan et al. reported a 58–72% reduction depending on CYP isoform and dosing regimen. Precision matters.
January 23, 2026 AT 07:00
Tatiana Bandurina
Let’s be honest - this whole post reads like a pharmacy textbook with a confidence complex. You list every drug carbamazepine messes with, but you never say what to do when the patient can’t afford alternatives or doesn’t have access to therapeutic drug monitoring. Most people aren’t in academic hospitals. They’re in rural clinics with one pharmacist on call. You’re diagnosing a problem but refusing to acknowledge the real world. That’s not helpful. That’s performative medicine.
January 25, 2026 AT 01:57
Philip House
Look, carbamazepine’s been around since the 60s. It’s not some newfangled drug. The fact that we’re still acting surprised by its enzyme induction is kind of embarrassing. We’ve known this for decades. If you’re prescribing it and you’re not checking levels, you’re not a doctor - you’re a liability. And yeah, the newer drugs are better, but they cost 10x more. So unless you’re rich or on Medicare, you’re stuck with the old-school stuff. Just don’t pretend it’s safe if you’re not monitoring. That’s all.
January 25, 2026 AT 20:09
Brenda King
Thank you for writing this. So many clinicians treat carbamazepine like it’s just another mood stabilizer. It’s not. It’s a metabolic wildfire. I’ve seen patients on lamotrigine for years, then get carbamazepine added for neuropathic pain - and suddenly they’re having seizures because their lamotrigine levels vanished. I always print out the interaction list and hand it to patients. I tell them: "This isn’t just about your seizure control - it’s about your life." And I always ask: "What else are you taking? Even that ginkgo or St. John’s wort?" 🙏
January 27, 2026 AT 04:53
Lana Kabulova
Wait - so if you stop carbamazepine and don’t adjust other meds, you can overdose on alprazolam? That’s terrifying. My aunt did exactly that. She was on carbamazepine for trigeminal neuralgia, stopped it cold turkey because her doctor told her to, kept her Xanax dose the same - ended up in the ER with respiratory depression. No one told her about the delayed reversal of enzyme induction. This needs to be screamed from the rooftops. Like, billboards. TV ads. EVERYONE needs to know this.
January 27, 2026 AT 20:33
arun mehta
As a pharmacist in rural Punjab, I can confirm: carbamazepine interactions are the #1 cause of medication errors in our clinics. Patients often come with 7–8 prescriptions from different doctors. No one talks to each other. We have to manually check every interaction. I’ve built a simple spreadsheet with the top 15 high-risk combos. I share it with every nurse. We call it ‘The Carbamazepine Death List.’ It’s saved lives. Also - yes, St. John’s wort is a silent killer here. Many patients think herbal = safe. It’s not.
January 29, 2026 AT 02:24
Patrick Roth
Okay but why is everyone acting like this is a new discovery? I remember in med school in 2012, our pharmacology professor said: "If you give carbamazepine to someone on a statin, you’re basically giving them a placebo." We’ve known this for 40 years. The real problem isn’t the science - it’s that lazy doctors don’t read the damn prescribing info. And now we’re writing essays about it like it’s groundbreaking? Wake up.
January 30, 2026 AT 22:58
Liberty C
How is this even still a thing? We have better options. We have safer, more predictable drugs. We have pharmacogenomics. And yet here we are - still forcing patients to navigate a minefield of enzyme induction because someone decided in 1968 that carbamazepine was "good enough." It’s not good enough. It’s archaic. It’s dangerous. It’s a relic of a time when we didn’t care enough to do better. If you’re still prescribing it without a genetic screen, a TDM plan, and a backup strategy - you’re not a clinician. You’re a dinosaur with a license.