MAO inhibitors are among the most powerful antidepressants ever developed-but they’re also some of the most dangerous if used carelessly. These drugs, first discovered in the 1950s, work by blocking an enzyme that breaks down key brain chemicals like serotonin, norepinephrine, and dopamine. That’s why they help people with severe, treatment-resistant depression. But the same mechanism that makes them effective can turn deadly when mixed with everyday medications, supplements, or even certain foods.
Why MAOIs Are So Risky
< p>MAOIs don’t just affect the brain. They affect your whole body. When you take an MAOI, your body loses its ability to safely process certain substances that normally get broken down by the monoamine oxidase enzyme. This includes not only prescription drugs but also over-the-counter cold remedies, herbal supplements, and even tyramine-rich foods like aged cheese or cured meats.The two biggest dangers are hypertensive crisis and serotonin syndrome. Hypertensive crisis happens when tyramine builds up in your blood, triggering a sudden, massive spike in blood pressure-sometimes over 200 mmHg systolic. That’s enough to cause a stroke, heart attack, or internal bleeding. Serotonin syndrome is even more insidious. It occurs when too much serotonin accumulates in your nervous system, leading to confusion, rapid heartbeat, fever, muscle rigidity, and in the worst cases, organ failure or death.
Medications That Can Kill You When Mixed with MAOIs
Many common prescriptions and OTC drugs are absolute no-gos with MAOIs. Here’s what you need to avoid:
- SSRIs like fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa). Combining these with MAOIs can trigger serotonin syndrome within hours. Even after stopping an SSRI, you must wait at least 14 days before starting an MAOI-and up to five weeks if you were on fluoxetine because it sticks around in your system so long.
- Dextromethorphan, the main ingredient in many cough syrups and cold pills. A single 30mg dose of this common OTC drug has caused fatal reactions in people on MAOIs. The FDA issued a warning in 1992, but many people still don’t realize it’s dangerous.
- Tramadol, meperidine, and methadone. These painkillers are especially risky. One 2019 case report described a 32-year-old man who ended up on a ventilator after taking tramadol while on selegiline.
- Linezolid, an antibiotic used for serious infections. It’s an MAOI itself. Taking it with another MAOI can cause serotonin syndrome. The FDA added it to the contraindicated list in 2006 after multiple deaths.
- Phenylephrine, found in Sudafed PE and many other decongestants. It causes dangerous spikes in blood pressure when combined with MAOIs.
- Ephedra and ephedrine-containing products. Even though the FDA banned most ephedra supplements in 2004, some still slip through. They’ve caused ICU admissions within 30 minutes of use in MAOI patients.
Supplements You Didn’t Know Were Dangerous
People often think “natural” means safe. That’s not true with MAOIs.
- St. John’s Wort-a popular herbal remedy for mild depression-can cause serotonin syndrome. One documented case involved a patient who developed a 40.5°C fever and blood pressure of 220/110 after taking it with phenelzine.
- 5-HTP and SAMe are sold as mood-boosting supplements. Both directly increase serotonin. Combining them with MAOIs is like pouring gasoline on a fire.
- Ginseng has been linked to mania and severe tremors in MAOI users. While some early cases might have been due to caffeine contamination, the risk is still real enough that doctors warn against it.
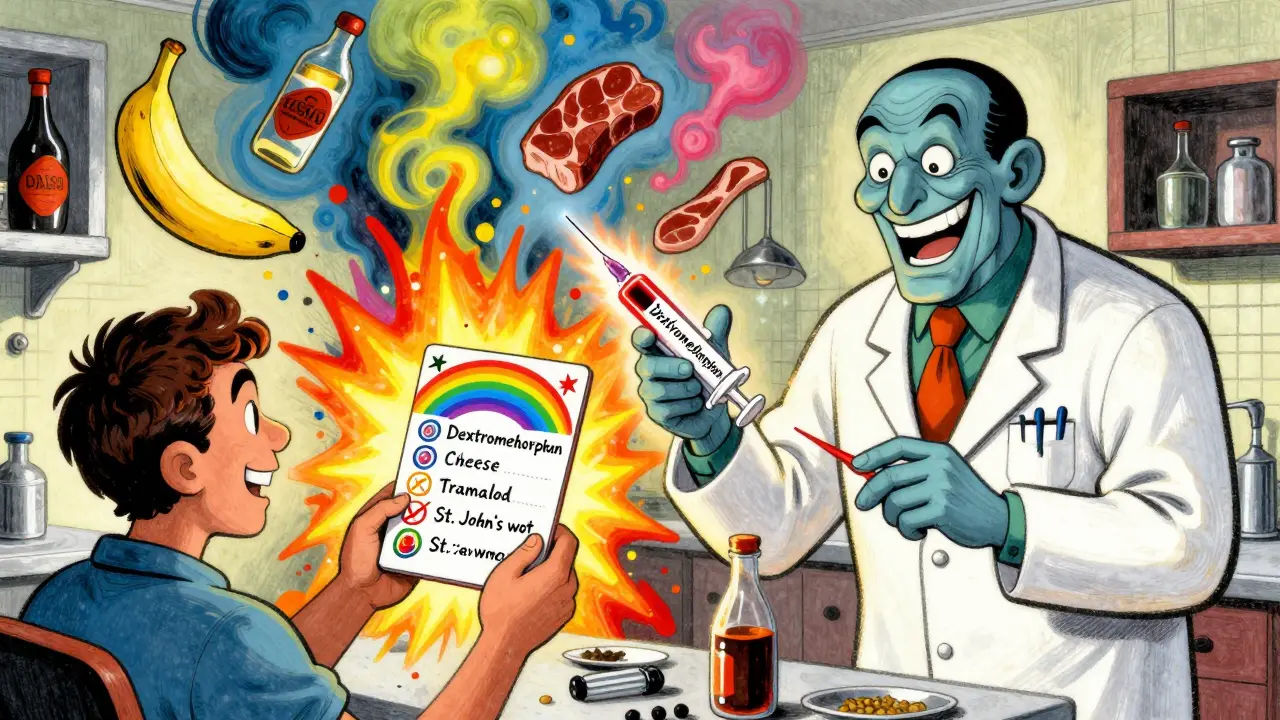
Food Risks Are Real-And Often Overlooked
Even if you avoid all medications, you can still trigger a hypertensive crisis from food. Tyramine builds up in aged, fermented, or spoiled proteins. Here’s what to skip:
- Aged cheeses (cheddar, blue, parmesan, Swiss-especially if stored over 6 months)
- Tap beer, draft beer, and some wines (Chianti, red table wine)
- Cured meats: pepperoni, salami, liverwurst, and summer sausage
- Soy sauce, miso, and other fermented soy products
- Overripe bananas, fava beans, and sauerkraut
It doesn’t take much. As little as 10-25mg of tyramine can trigger a crisis. One ounce of strong aged cheese contains about 15mg. That’s why even small portions matter.
There’s one exception: the selegiline patch (Emsam). At the lowest dose (6mg/24hr), it doesn’t block the enzyme in your gut the same way oral MAOIs do. That means you can eat tyramine-rich foods without restriction at this dose. But if you go higher, the dietary restrictions return.
What Happens When You Mix Them?
Imagine taking a cold medicine with phenylephrine while on phenelzine. Within 30 minutes, your blood pressure could jump from 120/80 to 220/110. You might get a pounding headache, blurred vision, chest pain, or nausea. If untreated, you could have a stroke or aortic dissection.
With serotonin syndrome, symptoms start subtly: shivering, diarrhea, restlessness. Then they escalate: high fever, muscle rigidity, seizures. Temperatures above 41.1°C (106°F) can cause kidney failure and rhabdomyolysis. Death rates in severe cases range from 2% to 12%.
These reactions don’t always happen immediately. Sometimes they build over days. That’s why many doctors miss them-especially in older patients on multiple meds.
How Doctors Are Trying to Prevent These Deaths
Since the 1990s, the FDA has required black box warnings on all MAOI labels-the strongest warning possible. In 2004, electronic health records were updated to block doctors from prescribing MAOIs alongside dangerous drugs. If you’re on an MAOI, your pharmacy system should flag any conflicting prescription before it’s filled.
Many psychiatrists now give patients wallet cards listing all contraindicated drugs. A 2020 survey found 78% of psychiatrists do this. But here’s the problem: primary care doctors often don’t know. A 2021 study showed 34% of family physicians didn’t realize dextromethorphan was dangerous with MAOIs.
Even with all these safeguards, mistakes still happen. People take OTC meds without telling their psychiatrist. Elderly patients see multiple doctors. Supplements aren’t tracked in medical records. And many patients don’t realize their cough syrup is a potential killer.
Is There a Safer Way?
Yes-sort of. The transdermal selegiline patch (Emsam) is now the most commonly prescribed MAOI in the U.S., making up 68% of all MAOI prescriptions in 2023. It’s easier to use, has fewer dietary restrictions at low doses, and causes fewer side effects. But it’s not risk-free. Higher doses still require strict food and drug avoidance.
Another option, moclobemide, is a reversible MAOI used in Europe and Canada. It’s much safer because it doesn’t permanently block the enzyme. But it was never approved in the U.S. because, in FDA trials, it wasn’t significantly better than placebo for severe depression.
So for now, if you’re on an MAOI, you’re stuck with caution. There’s no magic bullet. The only way to stay safe is to know what’s dangerous and avoid it completely.
What Should You Do If You’re on an MAOI?
- Carry a list of contraindicated drugs and foods in your wallet or phone.
- Tell every doctor, dentist, and pharmacist you’re on an MAOI-even for a simple procedure.
- Never start a new medication, supplement, or OTC product without checking with your psychiatrist.
- If you feel sudden headache, chest pain, fever, or confusion, go to the ER immediately.
- Don’t stop your MAOI abruptly. Talk to your doctor first.
MAOIs aren’t for everyone. But for some people-those who haven’t responded to dozens of other treatments-they’re life-changing. The key isn’t to avoid them entirely. It’s to use them with extreme care, full awareness, and total honesty with your care team.








January 23, 2026 AT 22:28
Luke Davidson
Man I never realized how many everyday things could blow up in your face on MAOIs. I had a friend who took NyQuil and ended up in ICU - he thought it was just a cold medicine, no big deal. Turns out it was dextromethorphan. Scary stuff. I’m telling everyone I know now.
January 25, 2026 AT 13:29
Karen Conlin
As someone who’s been on selegiline for three years, I can say this: the freedom of the patch at 6mg is life-changing. I eat blue cheese like it’s candy now. No more stress. But if you’re on oral MAOIs? Yeah, you gotta be a ninja. Write down every med, every supplement, every snack. I keep a laminated card in my wallet. No excuses.
January 25, 2026 AT 14:17
Patrick Gornik
Let’s be real - MAOIs are the last bastion of psychiatric alchemy. We’ve traded ancient, potent, terrifying tools for sanitized, corporate-approved SSRIs that make you feel like a zombie on a treadmill. The pharmaceutical industry doesn’t want you to know how powerful these drugs are - because they can’t patent the *danger*. The real tragedy isn’t the hypertensive crisis - it’s that we’ve become so risk-averse we’ve lost the capacity to treat the truly broken. Serotonin isn’t a bug, it’s a feature - and MAOIs are the scalpel that cuts through the noise. We’ve forgotten how to wield it.
January 26, 2026 AT 08:03
Dolores Rider
soooo… is it just me or does anyone else think the FDA is playing russian roulette with our meds? like… they knew about dextromethorphan since 92 but still let it sit on every drugstore shelf? and now they want us to trust their ‘black box warnings’? 🤡 i’ve seen people die from this. and no one gets punished. just another ‘oops’
January 27, 2026 AT 23:43
Heather McCubbin
MAOIs are the dark magic of psychiatry and honestly? I’m tired of people acting like they’re just ‘another antidepressant’. It’s not. It’s like driving a tank with no brakes and being told ‘be careful on the highway’. And now they want us to believe that ‘Emsam patch’ is safe? please. it’s just a slower version of the same suicide pact. My cousin took it and started hallucinating because she ate a banana. A BANANA. 😭
January 29, 2026 AT 05:56
Chloe Hadland
I’ve been on phenelzine for 5 years. I don’t eat cheese anymore, but I don’t miss it. What I miss is the peace. Before MAOIs, I couldn’t get out of bed. Now I teach yoga. I know the risks. I know the list. I carry it in my phone. And I’m alive. That’s worth the sacrifice.
January 29, 2026 AT 16:13
Jenna Allison
Just a quick note for anyone reading this: if you're on an MAOI and your doctor prescribes tramadol, say NO. Seriously. Even if they say ‘it’s just for a few days’. It’s not worth it. I’m a nurse and I’ve seen two patients go into serotonin syndrome from this combo. It’s not rare. It’s predictable. Ask for alternatives - gabapentin, acetaminophen, even physical therapy. There are options.
January 31, 2026 AT 09:51
Vatsal Patel
So let me get this straight - in America, you can buy a bottle of cough syrup that kills you if you’re on antidepressants… but you need a PhD to get a prescription for weed? 🤦♂️ This isn’t medicine. It’s performance art. We’re all just lab rats in a capitalist comedy of errors. Also, tyramine in cheese? Next they’ll ban air.
January 31, 2026 AT 22:37
Darren Links
MAOIs? Sounds like Soviet-era psychiatric horror. We used to have real medicine back in the day - not this ‘avoid cheese and pray’ nonsense. This is why America’s healthcare is broken. We let bureaucrats decide what’s safe instead of letting doctors use real tools. If you can’t handle the responsibility, don’t take the drug. Stop infantilizing adults. This isn’t a parenting class - it’s medicine.
February 1, 2026 AT 08:02
Amelia Williams
I’m so glad someone finally wrote this. I’ve been on Emsam for a year and honestly? It’s the only thing that worked. I used to cry every day. Now I hike, cook, even travel. I still avoid soy sauce and cold meds - but I don’t live in fear. Knowledge is power. And this post? It’s a gift. Thank you.
February 3, 2026 AT 02:06
Viola Li
Everyone’s acting like MAOIs are this mysterious danger, but honestly? It’s just laziness. If you can’t memorize a list of 10 foods and 7 drugs, maybe you shouldn’t be on a drug that can kill you. It’s not rocket science. Stop treating patients like children. If you can’t handle it, go back to Zoloft. No one’s forcing you to take this.
February 3, 2026 AT 17:21
asa MNG
wait so if i take a little bit of blue cheese and then take a cough drop… i’m basically playing russian roulette with my brain? 😳 i thought i was just being a foodie… now i’m scared to eat anything… also i just took a benadryl last week… oh god oh god oh god