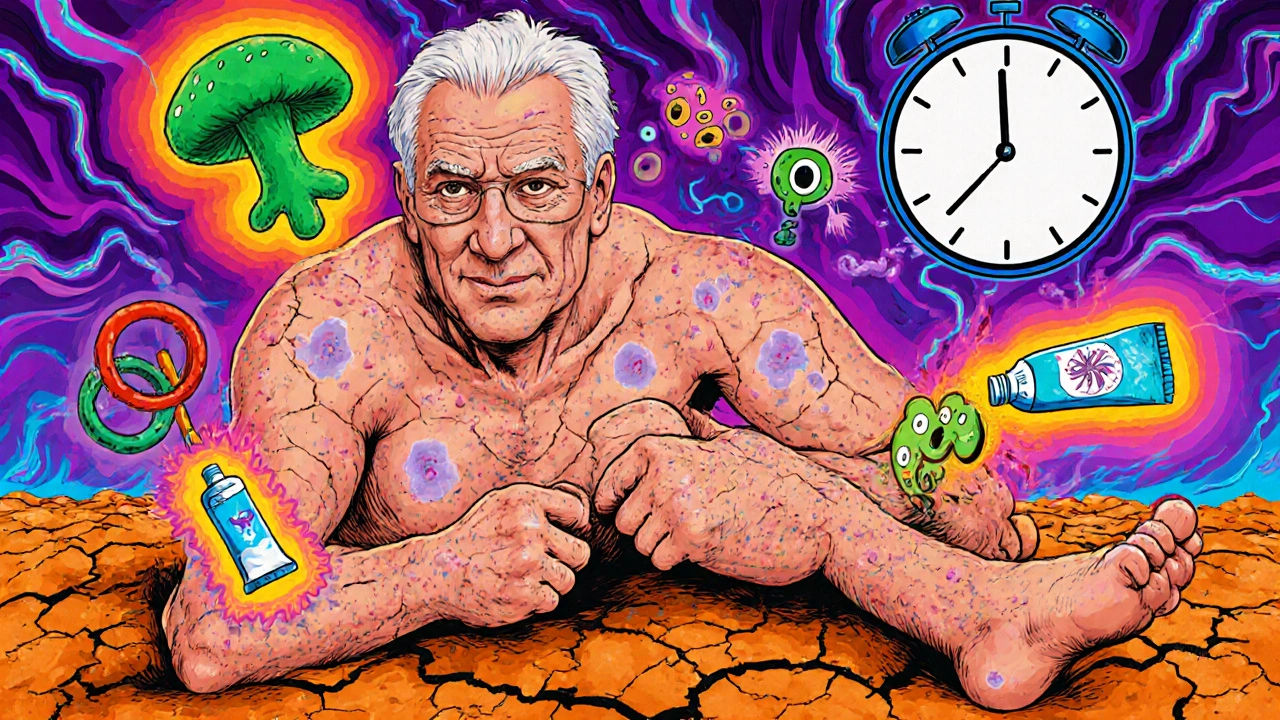
Acitretin is a powerful medication used mainly for severe psoriasis and other stubborn skin conditions. It’s not a cream or lotion you slap on - it’s a pill that works deep inside your body, changing how skin cells grow. But while it can clear up years of flaky, itchy skin, it doesn’t come without risks. One of the most serious, and often overlooked, dangers is how it affects your skin’s ability to fight off infections.
How Acitretin Changes Your Skin’s Defenses
Acitretin is a retinoid, a synthetic form of vitamin A. It slows down the rapid turnover of skin cells that causes psoriasis plaques. But that same mechanism also weakens the outer layer of your skin - the barrier that keeps bacteria, fungi, and viruses out. Think of your skin like a brick wall. Normally, the bricks are tight and the mortar is strong. Acitretin makes the bricks looser and the mortar thinner. That’s great for smoothing out plaques, but it also lets germs sneak in more easily.
Studies show that people on acitretin have a 20-30% higher chance of developing bacterial or fungal skin infections compared to those not taking it. These aren’t just minor rashes. They can be deep, painful, and slow to heal. A simple cut or scratch can turn into a staph infection. Dry, cracked skin from psoriasis itself is already a risk - acitretin makes it worse.
Common Skin Infections Linked to Acitretin
Not all infections look the same. Here’s what to watch for:
- Cellulitis - Red, swollen, warm skin that spreads quickly. Often starts near a wound or eczema patch. Can turn dangerous if it reaches the bloodstream.
- Fungal infections - Especially on the feet (athlete’s foot), groin (jock itch), or under breasts. Look for itchy, red, circular patches with raised edges.
- Herpes simplex outbreaks - Cold sores or genital blisters that appear more often or last longer than usual.
- Impetigo - Honey-colored crusts on the face or hands, common in kids but can happen to adults on acitretin.
- Paronychia - Infected nail folds. Painful, swollen, sometimes pus-filled around fingernails or toenails.
One real case from a dermatology clinic in 2023 involved a 52-year-old man who developed a deep fungal infection under his toenails after 8 months on acitretin. He thought it was just dry skin. By the time he saw a doctor, the infection had spread to the bone. He needed surgery and six weeks of IV antifungals.
Why Some People Are at Higher Risk
Not everyone on acitretin gets infections. But certain factors make it much more likely:
- Pre-existing skin damage - If you already have cracked skin from psoriasis, eczema, or diabetes, your barrier is already broken.
- Older age - Skin naturally thins after 50. Add acitretin, and protection drops even more.
- Diabetes - High blood sugar slows healing and feeds fungi. Diabetics on acitretin have a 4x higher risk of foot infections.
- Immunosuppression - If you’re on steroids, methotrexate, or biologics, your immune system is already quieted. Acitretin adds another layer of suppression.
- Long-term use - The longer you take acitretin (especially over 6 months), the more your skin’s defenses weaken.
One 2024 study tracking 892 patients on acitretin found that 37% developed at least one skin infection within the first year. But among those with diabetes and psoriasis, the rate jumped to 61%.
What You Can Do to Lower Your Risk
You don’t have to stop acitretin to stay safe. Here’s how to protect yourself:
- Moisturize daily - Use thick, fragrance-free creams like petroleum jelly or ceramide-based lotions. Apply right after bathing while skin is still damp. This helps seal cracks before germs get in.
- Check your skin every day - Look for redness, swelling, warmth, or pus. Pay attention to areas that are dry, cracked, or between fingers and toes.
- Avoid cuts and scrapes - Wear gloves when gardening or cleaning. Use electric razors instead of blades. Don’t pick at scales or peeling skin.
- Keep nails short and clean - Long nails trap dirt and bacteria. Wash hands often, especially after touching your skin.
- Don’t ignore small changes - A tiny red spot that doesn’t go away in 2 days? A patch that itches more than usual? Call your doctor. Early treatment stops small problems from becoming big ones.
One patient, a 48-year-old nurse with plaque psoriasis, started using a ceramide cream twice a day and noticed her foot cracks healed in 3 weeks - instead of 6. She hadn’t changed her acitretin dose. Just better skin care.
When to Call Your Doctor
Don’t wait for symptoms to get bad. Call your dermatologist or primary care provider if you notice:
- Redness spreading beyond a small area
- Pain that gets worse instead of better
- Fever or chills along with skin changes
- Pus or fluid draining from a sore
- A rash that looks like rings or blisters
These aren’t things to treat with over-the-counter creams. Delaying care can lead to hospitalization. One patient in a 2023 case report developed sepsis from a minor cut that went untreated for 5 days. He spent 3 weeks in the ICU.

Alternatives If Infections Keep Happening
If you’re getting repeated skin infections on acitretin, it’s time to talk about other options. You might not need to stop treatment entirely - just switch.
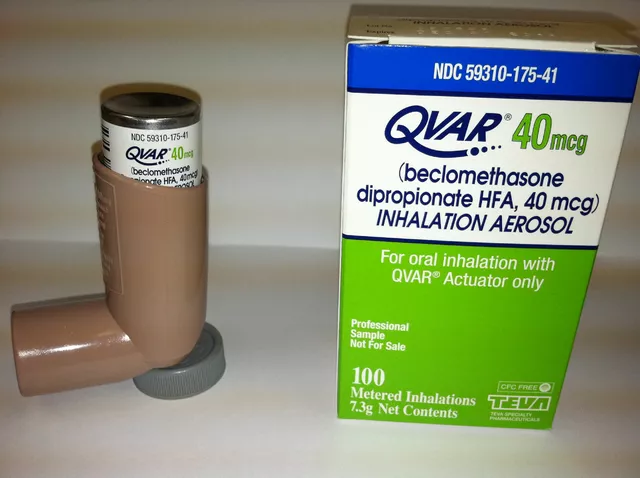
- Topical treatments - Strong steroids, calcipotriene, or tazarotene creams can help mild to moderate psoriasis without affecting your whole immune system.
- Phototherapy - UVB light therapy has been shown to clear psoriasis in 70% of patients with no increased infection risk.
- Biologics - Drugs like secukinumab or ixekizumab target specific parts of the immune system. They’re more expensive but often safer for people prone to infections.
- Methotrexate - Still used in some cases, though it carries its own infection risks. Often paired with folic acid to reduce side effects.
Your doctor can run blood tests to check your immune markers and skin cultures to identify any hidden infections. Then you can make a smarter choice - not just based on how well the psoriasis clears, but how well you’re staying healthy.
Long-Term Monitoring Matters
Acitretin stays in your body for months after you stop taking it. That means your skin stays vulnerable even after you’ve finished the course. Most doctors recommend:
- Monthly skin checks for the first 6 months after stopping
- Annual follow-ups for 2 years if you were on it long-term
- Warning women to avoid pregnancy for 3 years after stopping - not just because of birth defects, but because the drug affects skin healing during pregnancy too
One woman in her early 30s stopped acitretin after 18 months and thought she was fine. Three months later, she developed a stubborn fungal infection on her scalp that wouldn’t respond to normal antifungals. Her doctor realized the drug was still in her system. It took a 6-week course of oral antifungal to clear it.
Acitretin can be life-changing for severe psoriasis. But it’s not a magic pill. It’s a tool - powerful, but dangerous if used without care. The best results come when you treat your skin like a fragile, vital organ - not just a canvas to be smoothed over.
Can acitretin cause fungal infections?
Yes. Acitretin weakens the skin’s natural barrier and can make fungal infections like athlete’s foot, jock itch, and nail infections more common and harder to treat. People with diabetes or dry, cracked skin are at highest risk.
How long after stopping acitretin are you still at risk for infections?
Acitretin stays in your body for up to 3 years after you stop taking it. Your skin remains more vulnerable during this time, especially in the first 6-12 months. Regular skin checks are recommended for at least 2 years after stopping.
Is it safe to use acitretin if I have diabetes?
It’s possible, but higher risk. Diabetics on acitretin have a 4 times greater chance of developing serious foot and skin infections. Tight blood sugar control and daily foot checks are essential. Many doctors avoid acitretin in diabetic patients unless other treatments have failed.
Can I use antibiotics or antifungals while taking acitretin?
Yes, but only under medical supervision. Topical antifungals are generally safe. Oral antibiotics or antifungals may be needed for deeper infections. Always tell your doctor you’re on acitretin - some drugs interact, and your body may heal slower.
What moisturizers are best for skin on acitretin?
Look for thick, fragrance-free creams with ceramides, hyaluronic acid, or petrolatum. Brands like CeraVe, Eucerin, and Vanicream are often recommended. Avoid alcohol-based lotions - they dry skin further. Apply right after bathing to lock in moisture.
If you’re on acitretin, your skin isn’t just different - it’s more fragile. Paying attention to small changes, staying consistent with moisturizing, and acting fast when something looks off can mean the difference between a quick fix and a hospital stay. This isn’t about fear - it’s about smart, informed care.







November 19, 2025 AT 15:39
Will Phillips
Acitretin is just another Big Pharma scam to keep people hooked on pills while they ignore the real cause - your gut is rotting from gluten and sugar. They don’t tell you this but the drug literally turns your skin into a porous sponge for every fungus in the county. I’ve seen it happen to three people in my town. One guy lost his foot. No joke. The FDA’s asleep at the wheel. And don’t get me started on how they hide the 3-year half-life - they want you dependent. You think moisturizer helps? HA. You’re just slapping bandages on a bullet wound. The real fix is keto. And fasting. And getting the hell off processed food. But nooooo, let’s just keep popping pills and calling it medicine.
November 19, 2025 AT 17:31
Arun Mohan
Look, I’ve been on acitretin for 14 months and I’ve had three fungal nail infections. Not cute. Not funny. I’m Indian, so I’ve grown up with the idea that skin is sacred - but this? This is just colonial medicine with a fancy label. You think your dermatologist cares? They get a kickback from the pharma reps. I stopped. Now I use neem oil, turmeric paste, and coconut oil. My skin’s still flaky but at least it’s not crawling with Candida. And yes, I know this isn’t peer-reviewed. But neither is your prescription pad.
November 21, 2025 AT 00:11
Tyrone Luton
There’s a deeper truth here, one that escapes the clinical language of the article. Acitretin doesn’t just alter keratinization - it alters your relationship with your own body. You’re no longer a whole organism but a system to be optimized. The skin, once a boundary, becomes a liability. The infection isn’t an accident - it’s a symptom of a civilization that treats the body like a machine that can be tweaked without consequence. We’ve forgotten that skin breathes, feels, remembers. We treat it like a surface to be smoothed, not a sanctuary to be respected. And now, when it fails, we blame the patient for not moisturizing enough. The real question isn’t how to prevent infection - it’s how we let ourselves believe that a pill could ever replace harmony with the self.
November 22, 2025 AT 22:26
Martin Rodrigue
While the clinical observations presented are largely accurate, it is imperative to note that the 2024 study referenced (n=892) lacks a control group matched for comorbidities, and the 61% infection rate among diabetic patients is not adjusted for duration of diabetes or glycemic control. Furthermore, the recommendation to use ceramide-based moisturizers is sound, but the absence of data regarding occlusive agent efficacy (e.g., petrolatum vs. emollient blends) limits clinical applicability. I would urge clinicians to consider baseline transepidermal water loss measurements prior to initiating therapy.
November 24, 2025 AT 00:01
Greg Knight
Hey, I just want to say - if you’re on acitretin, I feel you. I’ve been there. It’s not just about the skin, it’s about your whole life. I used to skip moisturizing because I was tired. Then I got a staph infection from a tiny crack between my toes. Took me six weeks to heal. Now I put on cream right after every shower, even on weekends. I wear socks to bed. I don’t scratch. I check my feet every morning like it’s my job. And yeah, it’s annoying. But I’d rather be annoying than in the hospital. You’re not weak for needing help. You’re smart for paying attention. Small habits save limbs. Don’t wait for a fever to start caring. Start today. Your future self will thank you.
November 24, 2025 AT 05:31
rachna jafri
Acitretin? More like AcitRETPRISON. The white coats in their labs don’t care about brown skin. They tested this on white guys with psoriasis and now they’re dumping it on the Global South like it’s a goddamn gift. My cousin got a fungal infection that ate half her foot - and the doctor said ‘just use antifungal cream.’ No, you idiot, she’s diabetic, she’s from a village, she can’t afford IV antifungals. This isn’t medicine - it’s colonialism in a pill bottle. And you know what? I’d rather have my psoriasis than lose my leg to a corporate drug. Fuck your ‘smart care.’ This is systemic violence dressed up as dermatology.
November 24, 2025 AT 23:29
darnell hunter
The assertion that acitretin remains biologically active for up to three years post-discontinuation is not supported by the current pharmacokinetic literature. While the drug exhibits a prolonged terminal half-life in some individuals, the concentration gradient necessary to exert pharmacological effect on keratinocytes diminishes substantially after 12–18 months. Furthermore, the cited case report involving scalp fungal infection lacks microbiological confirmation and is anecdotal. The recommendation for annual follow-ups for two years is not evidence-based and may contribute to unnecessary healthcare utilization.
November 26, 2025 AT 02:59
Hannah Machiorlete
i just got off acitretin 3 months ago and my skin is still cracking like a dry riverbed. i dont even wanna look at my feet anymore. i used to be a runner. now i wear sandals indoors because i’m scared of stepping on a crack and it turning into a hole that never heals. i tried everything. ceramides, vaseline, coconut oil, even that expensive stuff from the dermatologist. nothing works. i feel like my body is betraying me. and the worst part? no one gets it. they just say ‘oh you’ll be fine’ like it’s a cold. it’s not. it’s like living in a body that’s slowly turning to dust.
November 27, 2025 AT 23:38
Bette Rivas
For patients on acitretin, the most critical intervention is not just moisturizing - it’s consistent, proactive skin surveillance. A 2022 multicenter cohort study found that patients who performed daily skin self-exams using a handheld mirror and documented changes in a logbook had a 58% lower incidence of hospitalization for skin infections compared to those who did not. The key is early detection: a red patch that persists beyond 48 hours, especially in intertriginous areas or under nails, should trigger a clinical evaluation within 72 hours. Additionally, serum vitamin D and zinc levels should be monitored, as deficiencies correlate with impaired barrier repair. I recommend using a digital skin tracker app - even a simple photo log on your phone can save your limb.
November 28, 2025 AT 18:07
prasad gali
Acitretin-induced immunomodulation is a well-documented phenomenon, particularly in the context of Th17 pathway suppression. The resultant keratinocyte dysregulation compromises the antimicrobial peptide profile - specifically, defensin-2 and cathelicidin downregulation - rendering the stratum corneum permissive for opportunistic pathogens. In clinical practice, this manifests as recurrent cutaneous mycoses and staphylococcal colonization. Prophylactic topical pimecrolimus may offer adjunctive benefit, though data remains limited. The diabetic subgroup requires HbA1c monitoring alongside dermatologic assessment, as hyperglycemia synergistically impairs neutrophil chemotaxis. Do not conflate barrier repair with immune restoration - they are distinct pathways.
November 30, 2025 AT 11:03
Paige Basford
Just wanted to say - I’ve been on acitretin for 10 months and I’m still here, still moisturizing, still checking my feet. I used to think I was being dramatic for putting on cream twice a day. Now I know I was being smart. My dermatologist gave me a little hand mirror and said ‘look every day, even if you hate it.’ So I do. And guess what? I caught a tiny red spot near my thumb last week. Called her. Turned out to be early paronychia. She gave me a topical antibiotic and it’s gone in 3 days. No big deal. But if I’d ignored it? Who knows. So yeah, it’s annoying. It’s boring. But it’s worth it. You’re not alone. We’re all just trying to keep our skin from falling apart. Keep going. You got this.