Statin Tolerance Risk Calculator
Find Your Statin Risk
This tool estimates your risk of statin-related muscle pain based on your SLCO1B1 genotype and the statin you're taking. Results are for informational purposes only.
Your Risk Assessment
Many people take statins to lower cholesterol and reduce their risk of heart attacks and strokes. But for some, the benefits come with a painful cost: muscle pain, weakness, or cramps. This isn’t just bad luck. For a growing number of patients, the problem isn’t the drug itself-it’s their genes.
Why Some People Can’t Tolerate Statins
Statin intolerance affects between 7% and 29% of users, with muscle-related side effects being the most common reason people stop taking them. Doctors often assume it’s just a side effect everyone experiences. But research shows something deeper is going on. A single gene variant, SLCO1B1, plays a major role in how the body handles certain statins-especially simvastatin. The SLCO1B1 gene makes a protein that pulls statins into the liver, where they’re broken down. If you have a specific change in this gene-called the c.521T>C variant, or rs4149056-your liver can’t clear the drug efficiently. That means more statin stays in your bloodstream, increasing the chance of muscle damage. People with two copies of this variant (CC genotype) are nearly five times more likely to develop severe muscle injury on high-dose simvastatin than those with no copies (TT genotype). Even one copy (TC) raises the risk by more than two times.Not All Statins Are Created Equal
This genetic risk isn’t the same for every statin. Simvastatin is the most affected. Atorvastatin and rosuvastatin? Much less so. A 2021 study of nearly 12,000 people found no meaningful link between the SLCO1B1 variant and muscle symptoms from atorvastatin or rosuvastatin. That’s why guidelines only recommend genetic testing before prescribing simvastatin, not other statins. If you’ve had muscle pain on simvastatin, switching to pravastatin or fluvastatin might solve the problem. These statins don’t rely as much on the SLCO1B1 transporter. One study showed that people with the high-risk CC genotype had 80% lower muscle side effects on pravastatin compared to simvastatin. That’s not just a small difference-it’s life-changing for someone who thought they couldn’t take any statin at all.What Other Genes Are Involved?
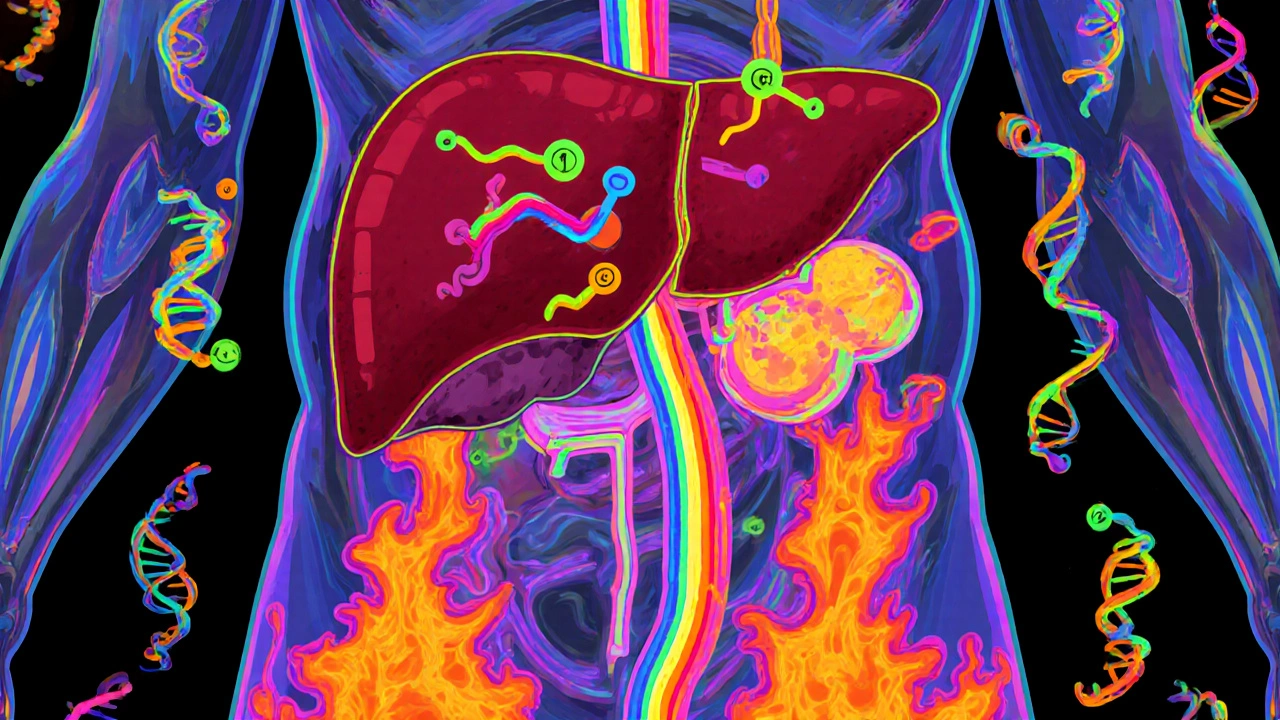
SLCO1B1 is the big player, but it’s not the only one. Other genes like CYP2D6, CYP3A4, ABCB1, and ABCG2 affect how statins are metabolized or pushed out of cells. Variants in these genes can change how much drug builds up in your muscles. One study even found a link between a variant in the GATM gene and muscle symptoms, though the exact reason is still unclear. And in 2021, researchers discovered a new candidate: SOAT1. Its role isn’t fully understood yet, but the statistical signal was strong enough to make it a serious focus for future research. Still, SLCO1B1 alone only explains about 6% of why people get muscle pain on statins. That means most cases aren’t caused by this one gene. Age, kidney function, thyroid issues, drug interactions, and even vitamin D levels matter too. Genetics is part of the puzzle-but not the whole picture.
When Should You Get Tested?
The Clinical Pharmacogenetics Implementation Consortium (CPIC) says testing for SLCO1B1 makes sense if you’ve had muscle symptoms on a statin and your doctor wants to try again. It’s not meant for everyone starting statins. The American College of Cardiology agrees: don’t test everyone, but consider it before re-challenging someone with simvastatin after intolerance. Some clinics test before the first prescription-called pre-emptive testing. A 2021 study found that people who got tested before starting any statin were 18.7% more likely to stick with therapy long-term. That’s because they avoided the trial-and-error phase. If you’ve had a family member with statin intolerance, or if you’re starting high-dose simvastatin (80 mg), pre-emptive testing might save you months of pain and frustration.How Testing Works
Getting tested is simple. A swab from your cheek or a blood draw is sent to a lab. Results come back in about a week. Companies like Mayo Clinic, ARUP, OneOme, and Color Genomics offer tests that include SLCO1B1 along with other relevant genes. The report will tell you your genotype-TT, TC, or CC-and what it means for your statin options. But here’s the catch: not all doctors know how to interpret the results. A 2021 survey found that 34% of primary care doctors felt unprepared to use this data. That’s why some labs include dosing recommendations right on the report. For example: “Avoid simvastatin 80 mg in CC genotype. Consider pravastatin 40 mg instead.” Electronic health records like Epic and Cerner now have built-in alerts. If a doctor tries to prescribe simvastatin 80 mg to a patient with a CC genotype, the system pops up a warning. That’s how you make pharmacogenomics practical in real clinics.Does Testing Actually Help?
The evidence is mixed. A 2020 trial published in JAMA Network Open gave SLCO1B1 results to doctors and patients-but found no improvement in statin adherence or muscle symptoms. That surprised many. But another study at Mayo Clinic showed that 78% of patients with prior statin intolerance were able to restart a statin successfully after genotype-guided switching. On Reddit, 62% of users reported better tolerance after testing. Why the difference? In the JAMA trial, doctors didn’t change prescriptions often enough. In the Mayo study, patients got clear guidance and support. The test isn’t magic-it’s a tool. It only works if someone uses it wisely.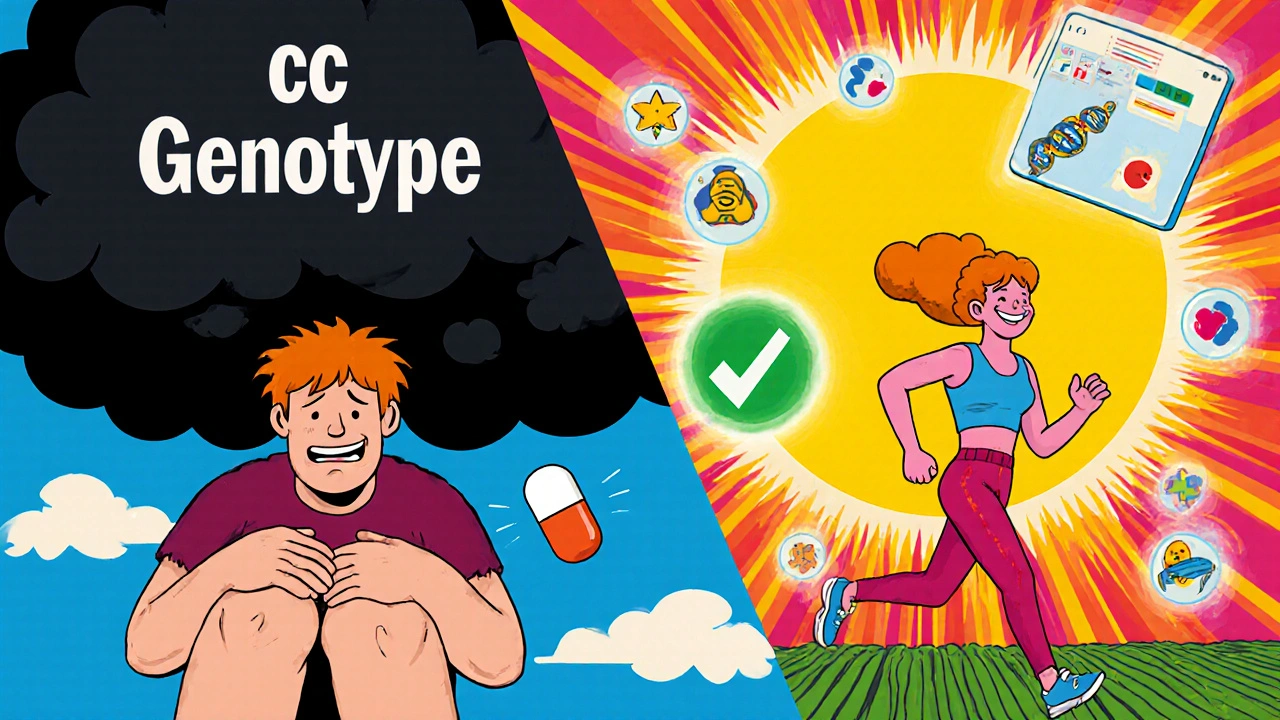
Cost and Insurance
Standalone SLCO1B1 testing costs between $150 and $400 out-of-pocket as of 2023. Insurance coverage is spotty. Only about 28% of commercial insurers covered it in 2022. Medicare rarely pays unless it’s part of a specific program. Some patients pay upfront and get reimbursed later. Others get it covered as part of a broader pharmacogenomic panel. If cost is a barrier, ask your doctor if the test is included in a hospital or research program. Some academic centers offer free testing for eligible patients.What’s Next?
Researchers are moving beyond single genes. New studies are building polygenic risk scores-combining SLCO1B1 with 10 to 15 other variants to better predict who’s at risk. Early results show these scores improve accuracy from 58% to 67%. That’s still not perfect, but it’s getting closer. By 2025, the Statin Pharmacogenomics Implementation Consortium plans to roll out standardized testing protocols across 50 U.S. hospitals. That’s a big step toward making this routine. The goal isn’t to stop people from taking statins. It’s to make sure they can take them safely. With over 35 million Americans on statins, even a small improvement in tolerance means thousands fewer heart attacks and strokes in the long run.Bottom Line
If you’ve quit statins because of muscle pain, don’t assume you can never take them again. Your genes might be the key. Ask your doctor about SLCO1B1 testing-especially if you were on simvastatin. If you’re high risk, switching to pravastatin or fluvastatin could let you keep the heart protection you need, without the pain. It’s not about avoiding medication. It’s about finding the right one for your body.Is pharmacogenomic testing for statins covered by insurance?
Coverage varies widely. As of 2023, only about 28% of commercial insurers cover standalone SLCO1B1 testing. Medicare rarely covers it unless it’s part of a specific molecular diagnostic program. Some employers or academic medical centers offer testing at no cost as part of research or preventive care initiatives. Always check with your insurer before testing, and ask your doctor if they can help you appeal a denial.
Can I get tested without a doctor’s order?
Yes, some direct-to-consumer companies like Color Genomics and 23andMe (through health add-ons) offer pharmacogenomic testing without a prescription. But these tests often lack clinical interpretation. Without a doctor or pharmacist reviewing your results, you might misinterpret your risk or miss important drug interactions. It’s safer-and more useful-to get testing ordered through a healthcare provider who can connect the results to your treatment plan.
Does SLCO1B1 testing work for all statins?
No. The SLCO1B1 c.521T>C variant has the strongest link to simvastatin-induced muscle injury. It shows little to no association with atorvastatin, rosuvastatin, or pravastatin. That’s why guidelines only recommend testing before prescribing high-dose simvastatin. If you’re on another statin and have muscle pain, SLCO1B1 testing is unlikely to explain your symptoms-but other factors like drug interactions or thyroid issues may be to blame.
What should I do if I have the high-risk CC genotype?
If you have the CC genotype, avoid simvastatin at 80 mg. Even lower doses carry increased risk. Instead, switch to a statin that doesn’t rely heavily on the SLCO1B1 transporter-like pravastatin, fluvastatin, or rosuvastatin. Studies show pravastatin reduces muscle side effects by 80% in CC carriers compared to simvastatin. Your doctor can adjust your dose and monitor your cholesterol to ensure you still get the heart protection you need.
How long does it take to get results from a pharmacogenomic test?
Most lab-based tests return results in 5 to 10 business days. Some hospitals with in-house labs can turn them around faster. Direct-to-consumer tests may take longer, up to 3 to 6 weeks, depending on shipping and processing. If you’re starting a new statin and need quick guidance, ask your doctor if they can order a rapid turnaround test.
Can pharmacogenomic testing prevent statin intolerance entirely?
No. SLCO1B1 explains only about 6% of statin-related muscle symptoms. Many other factors contribute-age, kidney function, other medications, low vitamin D, thyroid disease, and even physical activity levels. Testing helps avoid the most common genetic cause of intolerance, but it won’t eliminate all risk. Still, for those with the high-risk genotype, it’s the most effective way to prevent severe side effects and stay on therapy.
Are there any downsides to pharmacogenomic testing?
The main downsides are cost, limited insurance coverage, and the risk of misinterpretation. Some patients get results they don’t understand, leading to unnecessary worry or stopping effective treatment. Others pay out of pocket for a test that doesn’t change their care. Also, testing may reveal other genetic risks unrelated to statins, which can cause anxiety if not properly counseled. Always get testing through a provider who can explain the results in context.




November 17, 2025 AT 22:13
Jessica Healey
OMG I literally quit simvastatin after 3 weeks because my legs felt like concrete. My doctor just said 'it's normal' and shrugged. Turns out I'm CC genotype. Switched to pravastatin and now I run 5Ks without crying. Genetics saved my ass.
Why do docs act like this is new info??
November 19, 2025 AT 00:39
Levi Hobbs
Thank you for this incredibly well-researched post-it's rare to see such a nuanced take on pharmacogenomics. I work in clinical pharmacy, and I've seen firsthand how SLCO1B1 testing can prevent years of unnecessary suffering. The key isn't just testing-it's ensuring the results are integrated into the EHR with actionable alerts. Without that, it's just data sitting in a file.
Also, props for mentioning pravastatin and fluvastatin as alternatives. Too many clinicians default to 'just lower the dose' when switching statins is often the better path.
November 19, 2025 AT 03:56
henry mariono
Interesting. I’ve been on atorvastatin for 8 years with no issues. Never got tested. Maybe I’m TT? Or maybe my muscles just don’t care.
Still, good to know for people who struggle. I hope more docs start offering this before the first prescription.
November 20, 2025 AT 15:23
Sridhar Suvarna
As an Indian physician, I’ve seen patients from all genetic backgrounds. SLCO1B1 variant prevalence varies across populations-South Asians have higher frequency of the C allele than Europeans. But access to testing here is nearly nonexistent. Most patients pay out of pocket or never get tested.
This is not just a US problem. We need global equity in pharmacogenomics. Not just for statins, but for all high-risk drugs.
Let’s not make precision medicine a luxury for the wealthy.
November 22, 2025 AT 08:01
Joseph Peel
There's a fundamental disconnect here. We’re talking about a genetic variant that explains only 6% of statin intolerance, yet we’re treating it like a silver bullet. Meanwhile, we ignore the real culprits: poor diet, sedentary lifestyle, and polypharmacy.
Genetics is not an excuse to avoid lifestyle change. If you want to avoid statins, fix your cholesterol naturally first. Testing shouldn’t be the first step-it should be the last resort.
November 24, 2025 AT 01:32
Kelsey Robertson
Okay, but who funds these 'studies'? Pharma? Let’s be real-this is just another way to sell tests and keep people on brand-name drugs. Pravastatin? Generic. Rosuvastatin? Still expensive. They don’t want you to know you can just stop the statin entirely and take red yeast rice.
And don’t get me started on 'EHR alerts.' That’s just corporate surveillance dressed up as medicine.
They’re not helping you-they’re monetizing your fear.
November 24, 2025 AT 23:25
Joseph Townsend
Bro. I went from crying in the shower because I couldn’t lift my arms to biking 20 miles on pravastatin. This isn’t science-it’s a goddamn miracle. My doc didn’t even know what SLCO1B1 was until I printed out the paper and shoved it in his face.
Now I’m the guy in the waiting room handing out flyers. If you’ve quit statins because of pain? Get tested. Don’t let ignorance steal your life.
November 25, 2025 AT 12:20
Bill Machi
This is why America is falling apart. We’re out here running DNA tests instead of telling people to eat less sugar and move their bodies. We’ve turned medicine into a lottery where your genes determine your worth.
And now we’re paying $400 to find out you’re genetically 'weak'? That’s not medicine-that’s weakness culture. Get off the drugs. Work out. Stop blaming your DNA.
November 26, 2025 AT 04:52
Elia DOnald Maluleke
In the grand tapestry of human biology, we are but threads-each strand carrying the silent echoes of our ancestors. The SLCO1B1 variant is not merely a mutation; it is a whisper from the past, a molecular memoir of survival and adaptation.
Yet in our haste to quantify, to label, to test-we forget that the body is not a machine to be calibrated, but a symphony to be understood. The pain is real, yes-but so is the soul’s resilience.
Let us not reduce healing to a SNP. Let us remember: medicine must serve humanity, not the other way around.
November 26, 2025 AT 14:06
satya pradeep
Bro i got tested after my cousin had rhabdo on simvastatin. Turned out i was TC. switched to rosuvastatin and no issues. But here’s the thing-most docs in india dont even know this gene exists. Lab in delhi charged me 3k rupees. Worth it.
PS: if u have muscle pain and dont know ur genotype-just try pravastatin. cheap and safe. no need to wait for a test.
November 28, 2025 AT 04:16
Prem Hungry
Hey, if you're reading this and you've given up on statins because of muscle pain-you're not broken. You're just genetically different. And that's okay.
There's a statin out there for you. It might not be the first one your doctor pushed. But it's there.
Don't give up on your heart health. Just find the right key for your body. You deserve to live without pain and without fear.
And if your doctor doesn't know about SLCO1B1? Print this post. Bring it in. You've got this.
November 29, 2025 AT 16:57
Leslie Douglas-Churchwell
THIS IS THE NEW WORLD ORDER. They're testing your DNA to control your meds, then charging you $400 for the 'privilege' of being told what you can and can't take. Next they'll scan your microbiome to tell you which vegetables you're 'allowed' to eat.
And don't think for a second that your EHR alert isn't being sold to Big Pharma. They're not curing you-they're locking you into their ecosystem.
Ask yourself: Who benefits? Not you. Not your health. The algorithm. The corporation. The machine.
🧬💉 #PharmaControl #DontTrustTheTest