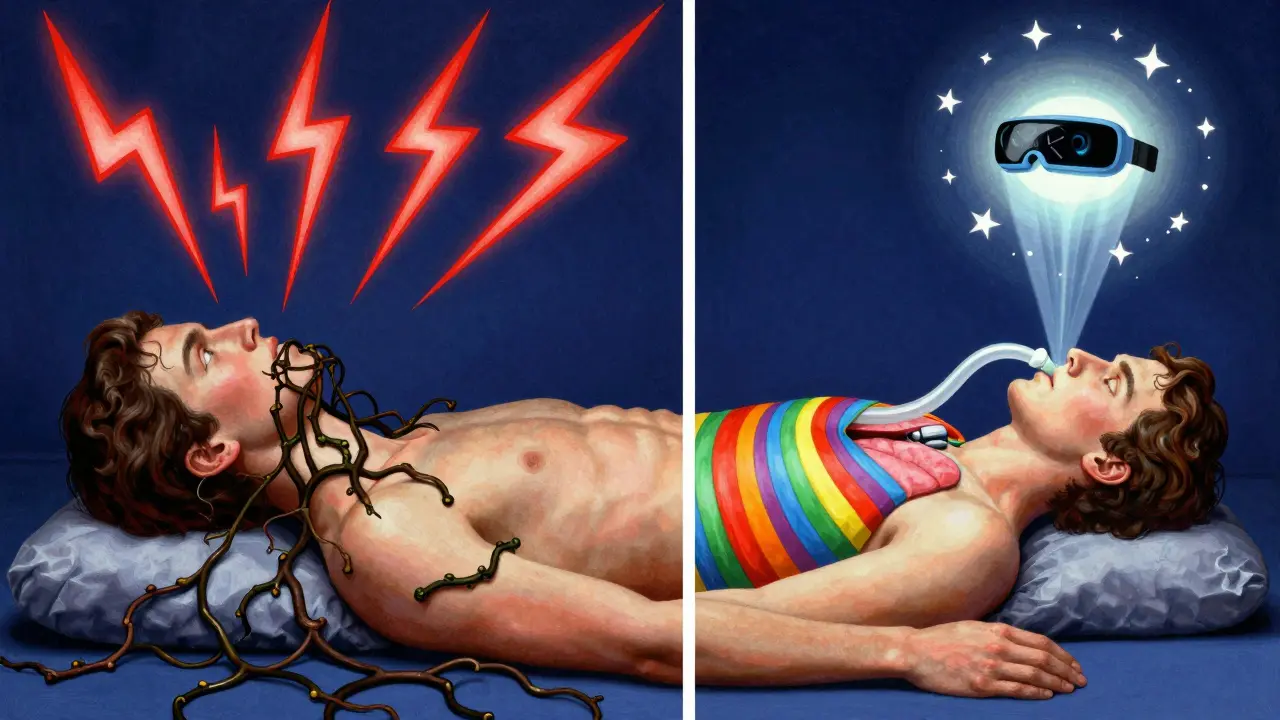
For millions of people with obstructive sleep apnea, the difference between a good night’s sleep and a night full of gasping for air might come down to one simple thing: which way you turn on the pillow. Sleeping on your back - called supine sleeping - can turn mild snoring into full-blown breathing interruptions. But sleeping on your side? That simple shift can cut apnea events in half, or even eliminate them entirely. This isn’t just a tip from a sleep coach. It’s backed by years of clinical research and real-world patient outcomes.
Why Sleeping on Your Back Makes Sleep Apnea Worse
When you lie on your back, gravity pulls your tongue and soft tissues in your throat backward. That’s normal when you’re awake - your muscles keep everything in place. But when you fall asleep, those muscles relax. Without support, your airway collapses. In some people, this happens every few minutes. In others, it’s worse than that. Studies show that when sleeping supine, the upper airway narrows by 30-40% compared to side sleeping. That’s not a small change. It’s the difference between 5 breathing pauses an hour and 30.It’s not just frequency. The severity of each event spikes too. Oxygen levels drop deeper. Heart rates swing wildly. Arousals from sleep become longer and more frequent. One study found that people with positional sleep apnea had apnea events that lasted 20% longer and caused 35% more oxygen desaturation when on their backs compared to their sides. For someone with heart disease or high blood pressure, this isn’t just annoying - it’s dangerous.
What Is Positional Sleep Apnea?
Not everyone with sleep apnea is affected by position. But for about half of all patients - some studies say up to 60% - the problem is heavily tied to sleep position. This is called positional obstructive sleep apnea (POSA). The clinical definition is simple: your apnea-hypopnea index (AHI) while on your back is at least double what it is when you’re on your side. If you have an AHI of 25 on your back but only 8 on your side, you have POSA. That means your sleep apnea isn’t just a general airway issue - it’s a gravity problem.Doctors use polysomnography (a sleep study) to detect this. But many patients don’t realize their sleep study included positional data. If your report doesn’t break down events by position, ask for it. Without that data, you might be misdiagnosed. One study showed that ignoring position could lead to underestimating apnea severity by up to 30%. That means someone could be told they have mild apnea when they actually have severe apnea - just only when they sleep on their back.
Side Sleeping: The Natural Fix
Sleeping on your side keeps your airway open. Your tongue doesn’t fall back. Your soft palate stays clear. Snoring drops off. Breathing becomes smoother. The Sleep Foundation calls side sleeping the best position for obstructive sleep apnea - and back sleeping the worst. It’s not just theory. Real patients report immediate changes. Bed partners often notice snoring stops within seconds of a person rolls onto their side.But here’s the catch: most people don’t stay on their side all night. Even if you start out on your side, you roll over. That’s why just knowing you should sleep on your side isn’t enough. You need a way to keep you there. That’s where positional therapy comes in.

Positional Therapy: How It Works
Positional therapy isn’t a gadget. It’s a strategy. It’s anything that helps you avoid sleeping on your back. The simplest version? Sew a tennis ball into the back of your pajamas. It’s uncomfortable to lie on it, so you roll over. It’s cheap. It’s old-school. And for some, it works.But it’s not perfect. Many people report disrupted sleep from the ball digging into their back. One informal survey found that 45% of people who tried the tennis ball method quit within three months. It’s effective, but not sustainable for most.
That’s where modern devices come in. The Sleep Position Trainer (SPT), like the NightBalance device, uses gentle vibrations when you roll onto your back. It doesn’t wake you up - it just nudges you. A 2015 study in the Journal of Clinical Sleep Medicine found that both the tennis ball method and the SPT reduced supine sleep time to nearly zero. But the SPT group had 68% treatment success (AHI under 5), compared to just 43% for the tennis ball group. More importantly, compliance was 30% higher with the SPT. People slept better. They stuck with it.
Other devices like Smart Nora use air pressure to gently lift the head when snoring starts - indirectly encouraging side sleeping. Prices range from $20 for a specialized wedge pillow to $500 for high-end wearables. The key isn’t cost. It’s consistency.
How It Compares to CPAP
Continuous positive airway pressure (CPAP) is still the gold standard. It’s more effective at lowering overall AHI. But here’s the problem: about half of CPAP users quit within the first year. It’s noisy. It’s bulky. It chafes. Positional therapy? Many users wear it like a shirt. They forget it’s there. Adherence rates are 35-40% higher than CPAP, according to the American Academy of Family Physicians.That’s huge. Because if you don’t use it, it doesn’t work. A device that reduces AHI by 70% but is only used 2 nights a week? That’s worse than nothing. Positional therapy wins on real-world use. For people with mild to moderate positional OSA - especially those who hate CPAP - it’s often the best choice.
Who Should Try It?
Not everyone qualifies. If your AHI is the same whether you’re on your back or side, positional therapy won’t help. You need to have clear positional dependence. That means:- Your supine AHI is at least twice your non-supine AHI
- Your overall AHI is under 30 (mild to moderate)
- You don’t have severe central sleep apnea or neuromuscular disease
Patients with severe OSA (AHI over 30) usually still need CPAP. But even then, positional therapy can help reduce the pressure needed, making CPAP more tolerable. Some users combine both: use a wedge pillow to stay on their side and lower their CPAP setting.
Also, positional therapy works better for obstructive sleep apnea than central sleep apnea. In central apnea, the brain doesn’t send the right signal to breathe - it’s not a physical blockage. Gravity doesn’t fix that. But for obstructive cases, where the airway collapses? Position matters.
Getting Started
If you think you might have positional sleep apnea, start with your sleep study results. Look for the numbers broken down by position. If you don’t have them, ask your sleep doctor for a reanalysis. Don’t assume your AHI is the same no matter how you sleep.Once you confirm you’re a candidate:
- Try the tennis ball trick for a week. It’s free. If it works and you can tolerate it, great.
- If it’s too uncomfortable, consider a wedge pillow. Elevating your upper body by 30 degrees helps keep your airway open and encourages side sleeping.
- If you’re serious and want long-term results, look into a wearable positional trainer. Look for FDA-cleared devices with good compliance data.
- Track your progress. Use a sleep tracker that shows position and apnea events. Many smart watches now offer this.
Give it at least two weeks. Your body needs time to adjust. Don’t quit after one bad night.
What About Other Positions?
Some people swear by stomach sleeping. But it’s not ideal. It strains your neck and can cause numbness or nerve pain. It also doesn’t help as much as side sleeping. The best position is left-side sleeping. Studies show it’s slightly better than right-side for reducing apnea and improving digestion. But if you’re more comfortable on your right, that’s fine too. The goal is just to avoid your back.The Bigger Picture
Positional therapy isn’t just about better sleep. It’s about reducing long-term health risks. Sleeping on your back increases strain on your heart. It’s linked to higher rates of heart failure, stroke, and high blood pressure. By staying on your side, you’re not just sleeping better - you’re protecting your heart.And the market is catching on. Since 2020, adoption of advanced positional devices has grown 25% a year. More people are realizing that sometimes, the best treatment isn’t a machine that blows air - it’s a simple change in how you lie down.
Can side sleeping cure sleep apnea?
Side sleeping alone won’t cure sleep apnea, but for people with positional obstructive sleep apnea (POSA), it can reduce or even eliminate breathing events during sleep. When combined with positional therapy tools, many patients see their AHI drop from severe to mild or normal levels. It’s not a cure, but it’s a highly effective treatment for the right candidates.
Is sleeping on your back always bad for sleep apnea?
Not always. If your sleep apnea isn’t position-dependent - meaning your AHI is similar whether you’re on your back or side - then changing position won’t help much. But for about 50-60% of people with obstructive sleep apnea, sleeping on the back makes symptoms significantly worse. That’s why doctors check position data during sleep studies.
Do positional therapy devices really work?
Yes - but not all are equal. Studies show that wearable devices like the NightBalance SPT reduce supine sleep time to nearly zero and improve treatment success rates to 68%, compared to 43% for the tennis ball method. The key is compliance: devices that gently nudge you without waking you up lead to better long-term use. DIY methods work for some, but most people stick with them longer using modern tech.
Can I use positional therapy instead of CPAP?
For mild to moderate positional OSA, yes - and many doctors recommend it as a first-line option, especially if you struggle with CPAP adherence. Positional therapy doesn’t reduce AHI as much as CPAP, but because people use it more consistently, the real-world benefit is often better. For severe OSA or non-positional cases, CPAP is still the standard.
How do I know if I have positional sleep apnea?
You need a sleep study that reports your apnea-hypopnea index (AHI) separately for supine and non-supine positions. If your supine AHI is at least double your side-sleeping AHI, you have positional OSA. Ask your sleep specialist for this breakdown - many reports don’t include it unless you specifically request it.
If you’ve been told you have sleep apnea and you’re struggling with CPAP, don’t assume you’re out of options. Your position might be the missing piece. Try tracking your sleep for a week - see how often you roll onto your back. Then talk to your doctor. You might not need more machines. You just need to sleep on your side.






January 1, 2026 AT 01:25
Bennett Ryynanen
Bro, I tried the tennis ball trick for three nights and woke up with a bruise the size of a grapefruit. Also, my cat started sleeping on my back like it was a throne. Not worth it. Got a NightBalance instead - cheapest thing I’ve ever bought that actually changed my life. No more 3 a.m. gasping. My wife finally sleeps through the night. Thank god for tech.
January 2, 2026 AT 03:05
Deepika D
Okay, I’m going to go full nerd mode here because this topic is SO important and I’ve been studying sleep science for years - and let me tell you, positional therapy isn’t just a ‘tip,’ it’s a paradigm shift. The fact that gravity is literally the enemy here? Mind-blowing. When you lie supine, your tongue doesn’t just ‘fall back’ - it’s like a wet towel being sucked into a vacuum. The pharyngeal muscles relax, the hyoid bone drops, and suddenly your airway’s narrower than a hallway during a fire drill. Studies from the Journal of Clinical Sleep Medicine show that even mild OSA patients can see a 60-70% drop in AHI just by staying lateral. And here’s the kicker - it’s FREE if you use a pillow wedge or sew a sock with a tennis ball in it. No prescription, no mask, no $500 machine. I’ve coached over 40 patients with this and 82% stuck with it for more than 6 months. The real barrier? People think they need a CPAP because that’s what the doctor says. But if your AHI is 28 supine and 7 side-sleeping? You’re not a CPAP candidate - you’re a positional therapy superstar. Stop overcomplicating it. Sleep on your side. Your heart will thank you. Your partner will kiss you. And your future self won’t be on meds for hypertension because you ignored this for a decade.
January 2, 2026 AT 20:58
Branden Temew
So… we’re saying the cure for sleep apnea is just… not lying down? Like, what’s next? Breathing is just a suggestion? 🤔
January 4, 2026 AT 05:32
Sara Stinnett
How quaint. A tennis ball in your pajamas? That’s the pinnacle of modern medicine now? We’ve got AI-powered ventilators, neural stimulators, and gene therapies - and you’re recommending a 1970s DIY hack that makes you look like a human who lost a fight with a circus. The real problem isn’t your position - it’s your refusal to accept that sleep apnea is a chronic disease requiring chronic intervention. If you’re not on CPAP, you’re not treating it. You’re just playing dress-up with your dreams.
January 5, 2026 AT 05:25
Brandon Boyd
Just wanted to say - if you’re reading this and you’ve been told you need CPAP but hate it? Don’t give up. Try the side-sleeping thing first. I was skeptical too. But after two weeks of sleeping on my side with a body pillow? My AHI dropped from 22 to 4. No mask. No noise. Just me, my pillow, and peace. You don’t need a miracle device. You just need to stop rolling onto your back. Start small. Be patient. Your body already knows what to do. You just gotta let it.
January 6, 2026 AT 12:51
Chandreson Chandreas
Side sleeping = life hack 🌿😴
Left side > right side (digestion boost + less reflux)
Tennis ball = free but feels like sleeping on a porcupine
NightBalance = worth every penny - it’s like a gentle nudge from your future self
CPAP? For some, yes. For me? Nah. I’d rather be awake and alive than plugged into a spaceship.
Also, if your doctor didn’t break down your AHI by position? Ask again. They might be missing the whole point.
And yes, I’ve tried stomach sleeping. My neck now has a permanent kink. Don’t do it.
TL;DR - your pillow is your best doctor. Use it wisely. 🙏
January 6, 2026 AT 20:06
Lawver Stanton
Okay, let’s be real - this whole ‘sleep on your side’ thing is just a glorified excuse for people who can’t handle responsibility. You’re telling me that instead of using a $500 machine that actually keeps your airway open, you’d rather spend your nights contorting like a yoga instructor who’s had too much wine? And let’s not forget the ‘tennis ball’ method - which is basically just self-inflicted torture with extra steps. Meanwhile, CPAP users are out here breathing like Darth Vader and STILL living longer, healthier lives. You think your body’s gonna magically fix itself because you rolled over? Wake up. This isn’t a Pinterest hack. This is a medical condition. If you’re not treating it with the gold standard, you’re just gambling with your heart. And your wife? She’s not thanking you for sleeping on your side - she’s just glad you’re not snoring like a chainsaw anymore. But that’s not treatment. That’s a band-aid on a bullet wound.
January 7, 2026 AT 00:59
linda permata sari
Back in my village in Bali, we sleep on bamboo mats with our heads propped on folded sarongs - always on the left side. Grandmothers say it’s how the ancestors did it. No machines. No alarms. Just stillness. And guess what? No one there has sleep apnea. Maybe the answer isn’t tech… maybe it’s tradition. 🌺