By early 2026, hospitals across the U.S. are quietly rationing life-saving medications. Antibiotics, insulin, cancer drugs - all in short supply. And it’s not because of a spike in demand. It’s because the pills and vials that once arrived reliably from factories in China, India, and Southeast Asia are stuck at ports, delayed by tariffs, or simply not being made at all. The root cause? A decades-long reliance on foreign manufacturing for the raw materials and finished products that keep Americans alive.
How Did We Get Here?
It started in the 1990s. Pharmaceutical companies saw a chance to cut costs. Making active pharmaceutical ingredients (APIs) in China or India was 70% cheaper than producing them in the U.S. Labor was cheaper. Regulations were looser. Factories could scale fast. By 2025, more than 80% of APIs used in U.S. medications came from abroad, with China alone supplying 40% of the total. The U.S. stopped building domestic API plants. Why build when you can buy cheaply from overseas? The system worked - until it didn’t. When the pandemic hit, global supply chains snapped. Lockdowns in Shanghai shut down factories making critical drug components. Shipping delays stretched from weeks to months. By 2024, the FDA reported 1,200 drug shortages - the highest number in a decade. And it wasn’t just one drug. It was dozens. Some were generic. Others were complex injectables. All of them depended on foreign production.Why Foreign Manufacturing Is a Risk for Medicines
Unlike smartphones or clothing, medicines can’t be easily swapped out. You can’t substitute one brand of insulin for another without risking patient safety. And unlike consumer goods, there’s no quick fix when a key ingredient disappears. The biggest problem? Concentration. A single factory in China might supply 90% of the world’s heparin. One plant in India makes 60% of the world’s generic antibiotics. If that factory has a power outage, a labor strike, or a regulatory shutdown, the ripple effect hits hospitals from New York to Nebraska. Add to that rising trade tensions. The U.S. imposed 12 new tariff categories on Chinese pharmaceutical inputs between 2024 and 2025. That didn’t stop imports - it just made them more expensive. Many manufacturers absorbed the cost. Others passed it on. Some just stopped ordering. Result? Empty shelves.The Numbers Don’t Lie
In 2025, U.S. business logistics costs hit $2.3 trillion - 8.7% of the entire national GDP. For pharmaceuticals, the numbers are even worse. Lead times from China to U.S. ports have increased by 50% since 2019. That means a shipment of raw material that used to take 20 days now takes 30. And that’s if it clears customs. Meanwhile, just-in-time inventory models - once praised for efficiency - became a liability. Many drugmakers kept only 15 to 30 days of inventory on hand. When a shipment got delayed, they had no buffer. By 2025, 56% of pharmaceutical companies reported cutting back on product offerings or delaying new drug launches because of supply chain issues, according to the National Foreign Trade Council. Even worse, 33% of companies managing global pharmaceutical supply chains say they’re understaffed. Finding people who understand both regulatory compliance and international logistics is hard. And cybersecurity? 60% of manufacturers say they’re worried about cyberattacks on their supply chain systems. A single ransomware attack on a supplier’s ERP system can halt production for weeks.What’s Being Done - And What’s Not Working
Some companies are trying to fix this. One Fortune 500 medical device maker switched from sourcing critical components from China to Mexico. Transportation costs dropped 35%. Lead times shrank from 45 days to 14. On-time delivery jumped to 99.2%. That’s the kind of win that’s possible. But not everyone can do that. Building a new API plant in the U.S. takes 18 to 24 months and costs 22% of your annual procurement budget. Most small and mid-sized drugmakers can’t afford that. And even if they could, the U.S. doesn’t have the skilled workforce to run these plants. There’s a shortage of chemical engineers, quality control specialists, and regulatory experts. The government has tried to help. The 2022 CHIPS and Science Act included funding for domestic pharmaceutical manufacturing. But most of that money went to semiconductors. Only 12% went to drug production. And the Inflation Reduction Act’s drug pricing provisions didn’t address supply chain vulnerability at all. Meanwhile, companies are turning to multi-shoring - spreading production across multiple countries. Instead of relying on China, they now source from India, Vietnam, and Poland. It’s expensive. It’s complex. But it works. Companies using this strategy saw 65% fewer disruption days in 2025 than those still tied to single-source suppliers.Why Reshoring Isn’t the Full Answer
Some politicians talk about bringing all drug manufacturing back to the U.S. But it’s not realistic. Wages for manufacturing workers in China are 4.8 times lower than in the U.S. for the same work. Rebuilding the entire supply chain domestically would raise drug prices by 30% to 50%. That’s not a solution - it’s a crisis. The real answer is balance. We don’t need to make everything here. We need to make sure we’re not putting all our eggs in one basket. We need to diversify. We need to build strategic stockpiles of critical drugs. We need to invest in digital tools - like AI-powered demand forecasting and blockchain for tracking ingredients - so we can see a disruption coming before it hits.
The Human Cost
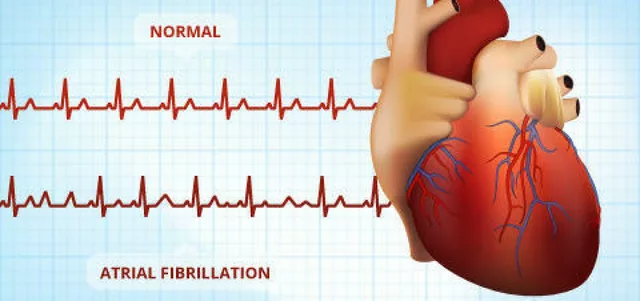
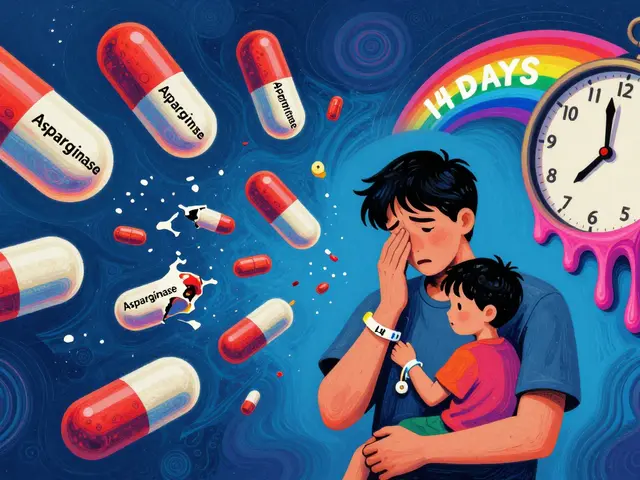
Behind every drug shortage is a patient. A diabetic who can’t get insulin. A cancer patient whose chemo is delayed. A child who can’t get antibiotics for pneumonia. In 2024, the FDA estimated that drug shortages contributed to over 2,000 preventable deaths in the U.S. That’s not a statistic. That’s a failure of policy, planning, and priorities. The companies that survived the worst of the shortages didn’t do it by luck. They did it by diversifying suppliers. They built inventory buffers. They moved production closer to home - not all the way, but enough to reduce risk. They invested in digital systems that gave them visibility into their supply chains. And they stopped treating manufacturing as a cost center - and started treating it as a lifeline.What You Can Expect Next
By 2027, the OECD predicts global GDP will recover slightly - if trade tensions ease. But for pharmaceuticals, recovery won’t come from luck. It’ll come from action. The U.S. is slowly starting to rebuild domestic API capacity. New plants are planned in Ohio, North Carolina, and Pennsylvania. The FDA is working with manufacturers to fast-track approvals for alternative suppliers. And more companies are adopting digital twins - virtual models of their supply chains - to simulate disruptions before they happen. But the biggest change? Mindset. The era of “cheapest is best” is over. The new rule is: “reliable is essential.”What Needs to Happen Now
If we want to stop drug shortages, we need three things:- Strategic stockpiles of critical drugs - not just for pandemics, but for everyday shortages.
- Government incentives for companies that diversify sourcing - tax credits, grants, and faster regulatory pathways.
- Investment in workforce training - we need more chemists, logisticians, and quality control experts who understand global supply chains.
Why are so many drugs made overseas?
Drugs are made overseas because it’s cheaper. Manufacturing active ingredients in countries like China and India costs up to 70% less than in the U.S. due to lower labor costs, fewer regulations, and established industrial infrastructure. Over the past 30 years, U.S. pharmaceutical companies shut down domestic plants and outsourced production to cut costs. By 2025, over 80% of active pharmaceutical ingredients (APIs) used in U.S. medications came from abroad.
Can the U.S. make its own drugs again?
Yes, but it’s expensive and slow. Building a single API manufacturing plant in the U.S. takes 18 to 24 months and costs about 22% of a company’s annual procurement budget. The U.S. also lacks enough trained workers - chemical engineers, quality control specialists, and regulatory experts - to run these plants at scale. While new plants are being planned in Ohio, North Carolina, and Pennsylvania, full domestic production isn’t realistic for all drugs. The goal isn’t to make everything here - it’s to make sure we have reliable backup sources.
How do tariffs affect drug shortages?
Tariffs don’t stop imports - they make them more expensive. Between 2024 and 2025, the U.S. imposed 12 new tariff categories on pharmaceutical inputs from China. Many manufacturers absorbed the cost, but others raised prices, cut back orders, or delayed shipments. Some suppliers stopped exporting to the U.S. altogether. This reduced supply without increasing domestic production, worsening shortages. In 2025, 75% of pharmaceutical companies reported that tariffs raised their operational costs, directly contributing to drug availability issues.
What’s multi-shoring, and how does it help?
Multi-shoring means spreading production across multiple countries instead of relying on one. Instead of getting all your APIs from China, you get some from India, some from Poland, and some from Mexico. This reduces the risk of a single disruption shutting down your entire supply chain. Companies using multi-shoring saw 65% fewer disruption days in 2025 compared to those still tied to single-source suppliers. It’s more complex and slightly more expensive, but it’s the most effective way to prevent shortages.
Why don’t drug companies just stockpile more medicine?
Many companies used to keep minimal inventory because it saved money - this is called just-in-time manufacturing. But when supply chains broke down, they had no buffer. Now, 71% of U.S. pharmaceutical companies are increasing inventory levels by 15% to 20%. The problem? Some drugs expire quickly. Others need special storage. Stockpiling isn’t simple. But it’s necessary. Strategic reserves for critical drugs - like insulin, epinephrine, and antibiotics - are now being considered by the FDA and HHS.
Is nearshoring to Mexico a good solution?
For many companies, yes. Shipping from Mexico to the U.S. takes 3 to 5 days instead of 30+ from Asia. Transportation costs drop by 30% to 40%. Labor is still cheaper than in the U.S., and regulatory alignment is easier under USMCA. One major medical device maker achieved 99.2% on-time delivery after shifting production to Mexico. But it’s not perfect - labor costs in Mexico are 15% to 20% higher than in China, and infrastructure isn’t always reliable. Still, it’s the best middle ground for many U.S. drugmakers.
What role does AI play in fixing drug supply chains?
AI helps predict disruptions before they happen. By analyzing shipping data, weather patterns, political events, and supplier performance, AI can flag risks weeks in advance. In 2025, 68% of large pharmaceutical companies used AI in their supply chains - up from 22% in 2020. Companies using AI-driven forecasting reduced stockouts by 40% and cut excess inventory by 25%. It’s not magic, but it’s the most powerful tool we have right now to make supply chains more resilient.
Are drug shortages getting better?
Slightly - but not enough. In 2025, global supply chain losses dropped to $184 billion, down from $1.5 trillion in 2022. That’s progress. But drug shortages remain at historically high levels. The FDA recorded over 1,200 shortages in 2024, and new ones are still being added. The difference now is that companies are more aware. More are diversifying. More are investing in tech. The trend is moving in the right direction, but we’re still playing catch-up - and patients are paying the price.