Switching from brand-name Coumadin to a generic version of warfarin sounds simple-cheaper, same drug, right? But for patients on warfarin, that switch isn’t just a pharmacy change. It’s a potential turning point in their health. Warfarin isn’t like taking an ordinary pill. It’s a warfarin with a razor-thin safety margin. Too little, and you risk a stroke or clot. Too much, and you could bleed internally. That’s why every single INR reading matters-and why switching generics isn’t something you do without a plan.
Why Warfarin Is Different
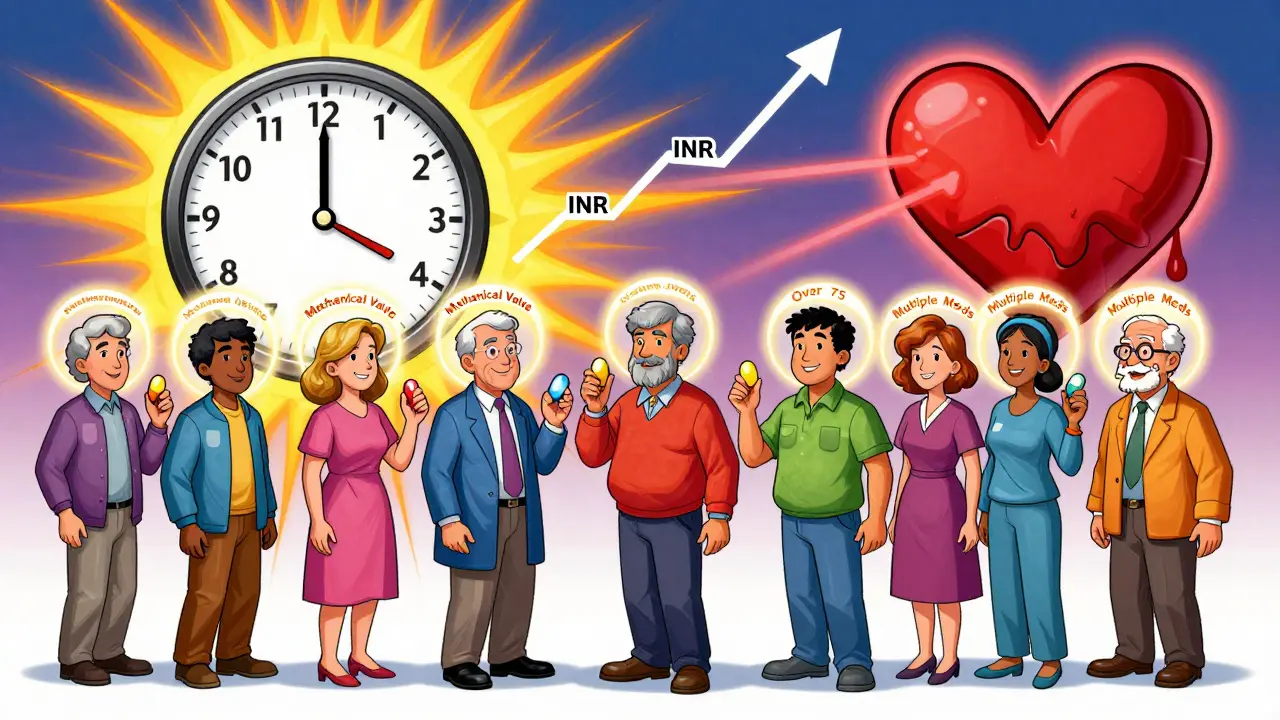
Warfarin has been around since the 1950s. It’s old, but it’s still essential. Millions of Americans take it to prevent clots after heart valve replacements, for atrial fibrillation, or after deep vein thrombosis. Unlike newer blood thinners like apixaban or rivaroxaban, warfarin doesn’t come with a fixed dose. You can’t just take one pill and forget it. Your blood’s clotting time-measured by the INR-must be checked regularly. The target? Usually between 2.0 and 3.0. For some, like those with mechanical mitral valves, it’s even tighter: 2.5 to 3.5.And here’s the catch: warfarin’s dose-response curve is unpredictable. A 5% change in dose can swing your INR out of range. That’s why it’s called a narrow therapeutic index drug. Even small differences in how your body absorbs the medication can tip the balance. That’s where generic switching becomes risky-not because generics are bad, but because they’re not all identical in how they behave in your body.
Generic Warfarin: Same Drug, Different Effects?
The FDA says all approved generic warfarin products are therapeutically equivalent to Coumadin. That’s based on bioequivalence standards: the amount of drug in your bloodstream (AUC) and peak concentration (Cmax) must fall within 80-125% of the brand. Sounds fine, right?But here’s what the FDA doesn’t say outright: those standards were designed for drugs with wide safety margins. Warfarin isn’t one of them. A 10% difference in absorption might be harmless for an antibiotic. For warfarin, it could mean the difference between a safe INR of 2.4 and a dangerous 3.8.
Studies tell a mixed story. A 2002 study tracking 182 patients in a St. Louis HMO found no increase in bleeding or clots after switching from Coumadin to Barr Laboratories’ generic warfarin. Another review of over 40,000 patients showed no major INR shifts on average. But averages don’t tell the whole story. In those same studies, some individuals saw their INR jump or drop by more than 1.0 point after switching-enough to trigger emergency care.
That’s why experts don’t say generics are unsafe. They say: watch closely when you switch.
When You Switch: The Monitoring Protocol
If you’re switching from Coumadin to a generic-or even from one generic brand to another-your INR needs to be checked more often. Not just once. Not just in a week. You need daily or every-other-day checks for the first 1-2 weeks.Why? Because it takes time for your body to stabilize. Your liver enzymes, your diet, even your sleep schedule can affect how warfarin works. A change in manufacturer can change how fast the pill dissolves. That changes absorption. That changes INR.
Here’s what your provider should do:
- Check INR the day before the switch (baseline).
- Check INR again within 24-48 hours after the first dose of the new generic.
- Check daily or every other day for the next 7-14 days.
- Once INR is stable for two consecutive readings, return to your regular schedule (every 4-6 weeks).
Some clinics even check INR at 3 weeks and 6 weeks after the switch, just to be sure. That’s not overkill-it’s standard practice at top anticoagulation centers.
What Can Throw Off Your INR After a Switch?
It’s not always the pill. But when your INR goes wild after switching generics, you need to rule out everything else first:- Diet changes: Eating a big salad or kale smoothie? Vitamin K counteracts warfarin. A sudden 100-150 mcg increase in vitamin K can drop your INR by 0.5-1.0.
- New medications: Antibiotics, aspirin, even some herbal supplements like garlic or ginkgo can boost warfarin’s effect. Over 300 drugs interact with it.
- Adherence: Missing a dose or taking two by accident? That’s a common cause of INR swings. About 20% of warfarin patients aren’t perfectly compliant.
- Lab error: Different labs use different methods. If you switched labs along with your pharmacy, that could explain the change.
If none of these explain the shift, then the generic switch is the likely culprit. And that’s when your doctor adjusts your dose-usually by 5-10%-and rechecks in a week.
Who’s at Highest Risk?
Not everyone needs extra monitoring. But some patients are more vulnerable:- Those with mechanical heart valves-especially mitral valves-where INR targets are stricter.
- Older adults, especially over 75, who metabolize drugs slower.
- People with liver disease or who take multiple medications.
- Patients who’ve had a previous clot or bleed on warfarin.
- Those switching between multiple generic brands (e.g., Teva to Mylan to Sandoz).
One study found that 15-20% of patients needed more frequent monitoring after switching generics. That’s 1 in 5 people. You can’t assume you’re in the 80% who glide through without issue.
Why Do Doctors Still Prescribe Warfarin?
If DOACs are easier, why not just switch everyone? Because warfarin still has advantages:- Cost: Generic warfarin costs $4-$10 a month. DOACs cost $300-$500.
- Reversibility: If you bleed, vitamin K or fresh frozen plasma can reverse warfarin within hours. DOACs need expensive, less available antidotes like idarucizumab or andexanet alfa.
- Long-term use in specific cases: Warfarin is still the only option for mechanical heart valves and antiphospholipid syndrome.
- Insurance coverage: Medicare and Medicaid often require step therapy-try warfarin first.
That’s why, in 2022, over 1.2 million Medicare beneficiaries were still on warfarin. And it’s why generic switching isn’t going away.
What You Can Do to Stay Safe
If you’re on warfarin and your pharmacy switches your pill:- Ask: Is this the same manufacturer as before? If not, request a copy of the pill’s imprint code or manufacturer name.
- Call your anticoagulation clinic or doctor immediately after the switch. Don’t wait for your next scheduled test.
- Keep a log: Note your INR, dose, diet changes, and any new meds.
- Don’t skip checks-even if you feel fine.
- Use the same pharmacy and lab consistently. Switching both at once makes it harder to track what’s causing changes.
Some clinics now use digital apps to track INR trends. If yours doesn’t, ask for one. Simple tools like MyINR or Anticoagulator can help you spot patterns before they become problems.
The Bottom Line
Generic warfarin is safe-for most people, most of the time. But safety isn’t automatic. It’s earned through attention. The data doesn’t show that generics are dangerous. It shows that switching without monitoring is dangerous.Warfarin doesn’t care if it’s called Coumadin or warfarin sodium. It only cares how much gets into your blood-and whether your INR stays in range. That’s why your doctor isn’t being overly cautious when they ask for extra tests after a switch. They’re doing their job.
If you’re stable on warfarin and your doctor suggests switching to generic to save money-go ahead. But don’t skip the follow-up. That one extra INR test might be the difference between a routine check-up and an emergency room visit.
Can I switch between different generic warfarin brands without checking my INR?
No. Even though all generics are FDA-approved as equivalent, switching between different manufacturers can cause unpredictable changes in your INR. Each brand may have slightly different fillers or manufacturing processes that affect absorption. Always check your INR within 48 hours of switching to a new generic brand, and continue daily or every-other-day monitoring for 1-2 weeks.
How often should I get my INR checked after starting warfarin?
When you first start warfarin, INR should be checked every 1-3 days until it’s stable. Once stable, you can extend checks to every 4-6 weeks. But if you switch generics, restart daily or every-other-day checks for 1-2 weeks-even if you’ve been on warfarin for years.
Is generic warfarin less effective than Coumadin?
No. Large studies show that generic warfarin is just as effective as Coumadin when used correctly. The difference isn’t in effectiveness-it’s in consistency. Some patients experience minor fluctuations in INR after switching, which is why close monitoring is required. The drug works the same; your body may respond slightly differently to each formulation.
Why do some doctors still prescribe Coumadin instead of generics?
Some doctors prefer Coumadin because they’ve seen more consistent results in their patients over decades. Others avoid switching patients unnecessarily to prevent INR instability. But cost and insurance rules often make generics the default. If you’re stable on Coumadin and don’t want to switch, you can ask your doctor to write "dispense as written" on the prescription.
Can I use a home INR monitor after switching generics?
Yes, if your doctor approves it. Home INR monitors are reliable and give you more control. But after switching generics, you should still coordinate with your provider. Don’t adjust your dose based on home results alone-call your clinic first. Home testing is great for tracking trends, but professional oversight is still essential during transitions.
What should I do if my INR is suddenly too high or too low after switching?
If your INR is above 4.5 or below 1.5, contact your doctor immediately. Do not change your dose on your own. For high INR, your doctor may pause your dose or give you vitamin K. For low INR, they may increase your dose. Always report any new symptoms-bruising, dark stools, headaches, or swelling-as these could signal bleeding or clotting.
Final Thought: It’s Not About the Pill-It’s About the Pattern
Warfarin therapy isn’t about finding the perfect pill. It’s about finding the right pattern: consistent diet, consistent dosing, consistent monitoring. Switching generics disrupts that pattern. And when you’re on a drug where a single point on the INR scale can mean life or death, you can’t afford to ignore the disruption.Generic warfarin saves money. But safety doesn’t come from the label-it comes from attention. Stay alert. Stay in touch with your care team. And never assume that "same drug" means "same effect." Your blood doesn’t care about the brand name. It only cares about the number on the screen.





December 26, 2025 AT 04:17
Christopher King
They don't want you to know this but the FDA is in bed with Big Pharma - they let generics slip through because they're paid off. Warfarin isn't just a drug, it's a control mechanism. The 'same drug' lie is how they keep you dependent. You think your INR is stable? It's not. They're manipulating your blood with invisible fillers. I've seen people bleed out after switching - and no one talks about it because the system is rigged.
They don't want you to ask questions. They want you to swallow the pill and shut up. But I'm not shutting up. This is chemical tyranny.
Wake up. Check your pill imprint. Cross-reference the manufacturer. Demand transparency. Or you'll be another statistic they bury under 'clinical guidelines.'
December 28, 2025 AT 00:49
Bailey Adkison
Warfarin is not a drug you switch without monitoring. That’s not opinion. That’s pharmacology. The narrow therapeutic index means even minor bioavailability differences matter. The FDA’s 80–125% bioequivalence window is inappropriate for anticoagulants. It was never designed for this. The data supports this. The studies prove this. Stop pretending it’s just a cost issue. It’s a safety failure disguised as efficiency.
December 28, 2025 AT 05:17
Michael Dillon
Look I get the concern but honestly most people switch generics and never have an issue. I’ve been on warfarin for 8 years and switched from Coumadin to Teva to Mylan three times. Never had an INR spike. My doc checks me every 6 weeks. I’m fine. Maybe it’s not as scary as they make it sound. People love to panic over pills. Chill out.
Also vitamin K isn’t some secret weapon. Eat your greens. Your INR will adjust. Stop treating your body like a broken calculator.
December 30, 2025 AT 04:54
Gary Hartung
Oh, the irony. A post about the 'razor-thin safety margin' of warfarin - written in a font that’s clearly Times New Roman, not the mandated Georgia for anticoagulant literature. The FDA’s guidelines, the CDC’s protocols, the ACC’s white papers - all meticulously documented - and yet here we are, in a Reddit thread where someone thinks 'generic' means 'identical.'
It’s not just the pill. It’s the entire infrastructure. The pharmacy’s storage conditions. The lab’s calibration. The nurse’s handwriting on the requisition. The entire system is a house of cards built on the delusion of standardization.
And you wonder why I don’t trust institutions.
December 31, 2025 AT 19:24
Ben Harris
I switched from Coumadin to a generic last year and my INR went from 2.6 to 4.1 in three days. I ended up in the ER. The pharmacist didn’t even tell me it was a different brand. I found out by looking at the pill. It was a different color. Smaller. No imprint code I recognized.
My doctor didn’t even apologize. He just said 'it happens.'
So now I take pictures of every pill. I log the lot number. I call the pharmacy before every refill. I don’t trust anyone. Not the doctor. Not the pharmacist. Not the FDA. Not even my own body anymore.
You think this is overkill? Try having a hemorrhage because someone thought 'same drug' meant 'same effect.'
And yes I know I’m dramatic. But my blood doesn’t lie.
December 31, 2025 AT 23:55
Jason Jasper
I’ve been on warfarin for 12 years. Switched generics twice. Both times my INR was stable after the first check. I think the key is communication. Talk to your provider. Don’t assume. Don’t panic. But don’t ignore it either. I use a home monitor now - it gives me peace of mind. The system isn’t perfect, but it’s not a conspiracy either. Just a drug that needs care.
Don’t let fear make you distrust everything. Stay informed. Stay calm. Stay consistent.
January 2, 2026 AT 22:36
Mussin Machhour
Guys I just want to say - if you're on warfarin and you're worried about switching generics, you're not alone. I used to freak out every time my pharmacy changed the pill. But I started keeping a simple notebook - INR, dose, what I ate, how I slept. After a few months I started seeing patterns. Turns out my INR was more affected by my weekend pizza than the generic switch.
Don't stress the pill. Stress the pattern. And if you're unsure? Just call your clinic. They'll tell you what to do. Seriously. They're there to help.
January 4, 2026 AT 11:42
Linda B.
Of course the FDA says generics are safe. They also said thalidomide was fine for morning sickness. And cigarettes were harmless. And asbestos was a miracle material. The system doesn’t protect you. It protects profit.
They don’t want you to know that the same pill can be made in three different countries with three different binders - and none of them are tested on people with your exact liver enzymes.
So go ahead. Trust the label. I’ll be the one with the home monitor and the emergency vitamin K vial.
January 4, 2026 AT 16:12
Carlos Narvaez
Warfarin isn’t like insulin. It’s not a replacement. It’s a balancing act. The brand name doesn’t matter. The consistency does. If you switch, monitor. If you don’t monitor, you’re gambling. Simple.
Stop turning a clinical protocol into a moral crusade. It’s medicine. Not a dystopian novel.
January 4, 2026 AT 22:51
Lindsay Hensel
As someone who works in anticoagulation clinics across three states, I can confirm: the protocol outlined here is gold standard. Daily INR checks for two weeks after a switch? Non-negotiable.
Patients who skip it? They end up back in the hospital. Sometimes with catastrophic outcomes.
This isn’t fearmongering. It’s clinical reality. And if your provider isn’t following this - ask why. Push back. Your life depends on it.
Thank you for writing this. It’s needed.
January 5, 2026 AT 18:16
Oluwatosin Ayodele
You Americans overthink everything. In Nigeria we use warfarin generics every day. No one checks INR daily. We check once a month. People live. People thrive. You have too many doctors. Too many tests. Too many pills. Just take the medicine. The body knows what to do.
Stop treating warfarin like a magic potion. It’s a tool. Use it. Don’t worship it.
January 5, 2026 AT 20:12
Terry Free
Let’s cut through the noise. The data says 80% of patients are fine after switching. The other 20%? They’re the ones who skip INR checks. Or they eat kale every day. Or they take ibuprofen. Or they miss doses. Don’t blame the pill. Blame the behavior.
Warfarin isn’t fragile. It’s the patients who are inconsistent. Fix the habits. Not the pharmacy.
January 7, 2026 AT 12:18
sagar patel
Switched generics last month. INR was 2.8 before. 2.9 after. No drama. No ER. No panic. Just a pill. Just a number. Just life. Stop turning medicine into a horror movie.