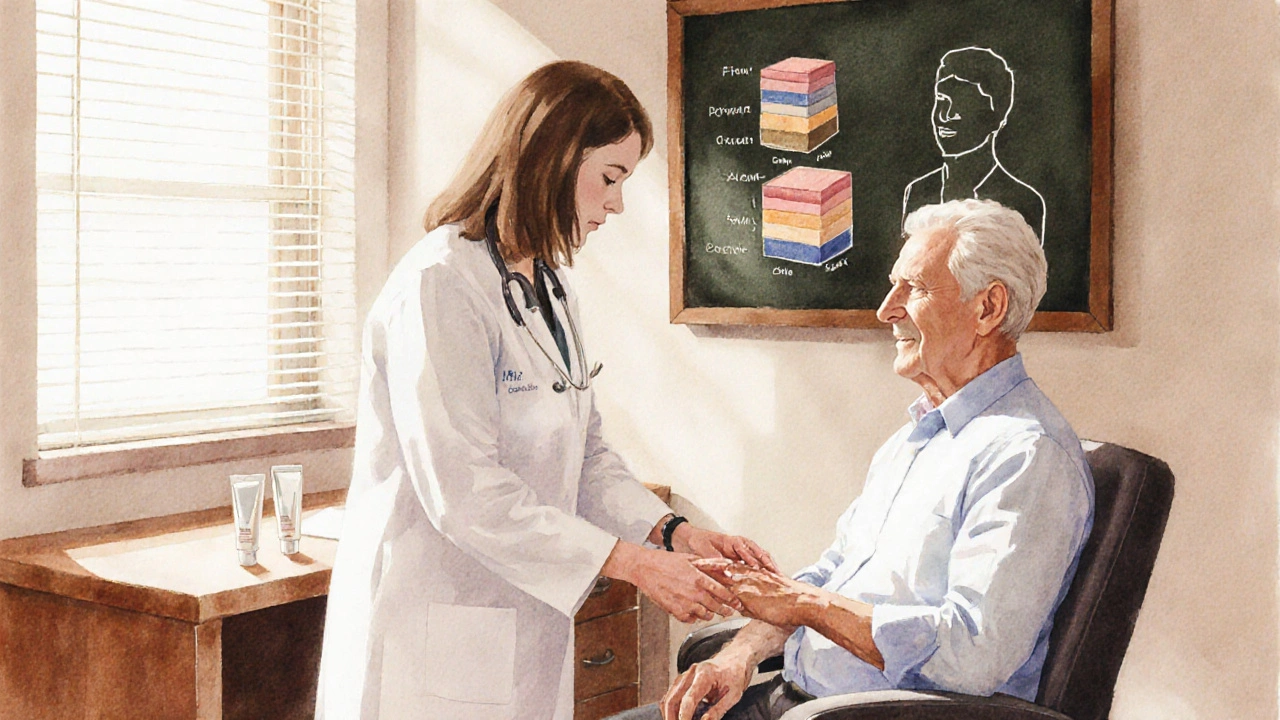
Topical Steroid Potency & Usage Guide
Recommended Treatment:
Important Notes:
| Medication | Potency | Best For | Common Side Effects |
|---|---|---|---|
| Temovate (Clobetasol) | Super-High | Severe psoriasis, lichen planus | Atrophy, striae, HPA suppression |
| Halobetasol | Super-High | Chronic plaque psoriasis | Atrophy, burning |
| Betamethasone | High/Medium | Eczema, dermatitis | Skin thinning, irritation |
| Triamcinolone | Medium | Allergic contact dermatitis | Mild thinning, redness |
| Hydrocortisone | Low | Mild irritations, periorbital skin | Minimal |
| Tacrolimus | Non-steroid | Atopic dermatitis, steroid-sparing | Burning, itching (initial) |
When managing tough skin conditions like psoriasis or eczema, many patients reach for a powerful steroid cream. Temovate (Clobetasol propionate) is one of the strongest topical corticosteroids available, but it isn’t the only option. Knowing how it stacks up against other treatments can save you from unnecessary side effects and help you pick the right strength for your skin.
Key Takeaways
- Temovate is a super‑high‑potency steroid; use it only for short periods on limited areas.
- Halobetasol and Betamethasone provide similar potency with slightly different irritation profiles.
- Medium‑potency steroids like Triamcinolone work well for moderate flares and have a lower risk of skin thinning.
- Non‑steroid options such as tacrolimus or pimecrolimus are useful for steroid‑sparing strategies.
- Choosing the right product depends on potency, location of the rash, duration of treatment, and personal tolerance.
What Is Temovate?
Temovate belongs to the class of super‑high‑potency topical corticosteroids. Its active ingredient, Clobetasol propionate, penetrates deep into the skin to suppress inflammation, reduce redness, and slow the over‑production of skin cells.
Typical uses include:
- Severe plaque psoriasis
- Lichen planus
- Chronic hand eczema that hasn’t responded to milder steroids
Because of its strength, the drug is usually prescribed for a maximum of two weeks on any one body area. Over‑use can lead to skin atrophy, telangiectasia, or systemic absorption.
Major Alternatives to Temovate
Below are the most common prescription‑strength alternatives, each with its own potency level and safety profile.
Halobetasol (Halobetasol propionate) is a super‑high‑potency steroid that is often marketed as a “once‑daily” option for plaque psoriasis and chronic dermatitis.
Betamethasone (Betamethasone dipropionate) comes in various strengths; the 0.05% cream is considered high potency, while the 0.025% lotion is medium potency.
Triamcinolone (Triamcinolone acetonide) is a medium‑potency steroid widely used for eczema, allergic contact dermatitis, and insect bites.
Hydrocortisone (Hydrocortisone acetate) is a low‑potency steroid available over‑the‑counter, suitable for mild irritations and periorbital skin.
Tacrolimus (Tacrolimus ointment) is a non‑steroidal calcineurin inhibitor used for atopic dermatitis when steroids are unsuitable.
Pimecrolimus (Pimecrolimus cream) works similarly to tacrolimus but is formulated for sensitive areas like the face.
Moisturizer (Emollient cream or ointment) isn’t a drug, but daily use can reduce the need for steroids in many chronic conditions.

Side‑Effect Profile Across Options
All topical steroids share a core set of possible side effects, but the risk escalates with potency and duration.
- Skin thinning (atrophy): Most common with super‑high‑potency agents like Temovate and Halobetasol.
- Stretch marks (striae): Usually appear after weeks of continuous use on large areas.
- Hypopigmentation: Lightening of skin is more visible on darker complexions.
- Systemic absorption: Rare, but can suppress the hypothalamic‑pituitary‑adrenal axis in extensive or occluded applications.
- Non‑steroid alternatives (tacrolimus, pimecrolimus) may cause burning or itching at the start of treatment, but they don’t cause atrophy.
Comparison Table
| Medication | Potency | Prescription? | Best For | Frequent Side Effects |
|---|---|---|---|---|
| Temovate | Super‑high | Yes | Severe psoriasis, lichen planus | Atrophy, striae, HPA suppression |
| Halobetasol | Super‑high | Yes | Chronic plaque psoriasis | Atrophy, burning |
| Betamethasone | High (0.05%) / Medium (0.025%) | Yes | Eczema, dermatitis | Skin thinning, irritation |
| Triamcinolone | Medium | Yes | Allergic contact dermatitis | Mild thinning, redness |
| Hydrocortisone | Low | No (OTC) | Mild irritations, periorbital skin | Minimal |
| Tacrolimus | Non‑steroid | Yes | Atopic dermatitis, steroid‑sparing | Burning, itching (initial) |
| Pimecrolimus | Non‑steroid | Yes | Facial eczema, sensitive skin | Burning, itching (initial) |
How to Choose the Right Option for You
Follow this decision flow to match potency with the condition:
- Assess severity. If the rash is intense, thick, or covers less than 10% of body surface, a high‑potency steroid like Temovate or Halobetasol may be justified.
- Identify location. Sensitive areas (face, groin, armpits) demand lower‑potency or non‑steroid treatments.
- Set treatment length. Plan to taper down after 2‑4 weeks for high‑potency steroids; longer use signals a need to switch to medium‑potency or steroid‑sparing agents.
- Consider comorbidities. Diabetes, osteoporosis, or immune suppression can increase risks from systemic absorption-favor milder options.
- Trial a steroid‑sparing agent. For chronic eczema, start with tacrolimus or pimecrolimus, adding a short burst of a low‑potency steroid if flare‑ups occur.
Always discuss the plan with a dermatologist, especially when using super‑high‑potency steroids on children.
Practical Tips & Common Pitfalls
- Apply a thin layer. Rub the cream in gently; a pea‑size amount per palm-sized area is usually enough.
- Avoid occlusion unless directed. Covering the treated area with plastic wrap can dramatically increase absorption and side‑effects.
- Rotate products. Switching from a high‑potency steroid to a medium‑potency or non‑steroid after a few weeks reduces the chance of atrophy.
- Monitor skin changes. Look for thinning, stretch marks, or new bruising. If you notice any, stop the product and see a clinician.
- Don’t use on infected skin. Bacterial or fungal infection requires antimicrobial treatment first.
Frequently Asked Questions
Can I use Temovate on my face?
Generally, no. The skin on the face is thin and more prone to atrophy. If a facial rash needs a steroid, doctors usually prescribe a low‑potency option like hydrocortisone or a non‑steroid such as tacrolimus.
How long is it safe to stay on Temovate?
Most guidelines limit continuous use to 2‑4 weeks on any single body area. After that, a taper to a lower‑potency steroid or a steroid‑sparing agent is recommended.
Is Halobetasol stronger than Temovate?
Both are classified as super‑high‑potency steroids, so their anti‑inflammatory power is comparable. Individual response and irritation potential may differ, so some clinicians prefer one over the other based on patient tolerance.
When should I switch to a non‑steroid like tacrolimus?
If you need long‑term control of atopic dermatitis, have frequent steroid‑related side effects, or are treating delicate areas, a calcineurin inhibitor is a safer choice for maintenance therapy.
Can I buy any of these steroids over the counter?
Only low‑potency hydrocortisone (usually 0.5% to 2.5%) is available without a prescription in most U.S. states. All higher‑potency creams, including Temovate, Halobetasol, Betamethasone, and Triamcinolone, require a doctor’s order.
Next Steps
If you suspect you need a high‑potency steroid, schedule a dermatology appointment. Bring a list of current medications and any history of skin thinning. Ask your doctor to outline a clear tapering plan and to discuss whether a steroid‑sparing agent could keep your skin healthy long‑term.






October 6, 2025 AT 12:49
TRICIA TUCKER
Hey folks, great rundown on the steroid ladder! If you’re new to this, think of it like a coffee order – the stronger the brew, the quicker the buzz, but also the higher the chance of a crash. Start low, watch how your skin reacts, and only crank it up if you really need that extra kick. And don’t forget the moisturizer – it’s the unsung hero that keeps the whole thing from turning into a desert.
October 7, 2025 AT 17:13
Dave Tu
While the article enumerates the options, it neglects to mention that the over‑prescription of super‑high‑potency steroids like Temovate often serves pharmaceutical interests more than patient welfare. The safety profile is not as benign as portrayed; systemic absorption can subtly suppress the HPA axis, a fact routinely downplayed in clinical guidelines.
October 8, 2025 AT 21:00
Johnna Sutton
Upon careful examination, one must acknowledge the hidden agenda behind the promotion of Temovate. The elite medical establishment, in collusion with big pharma, deliberately obscures the fact that long‑term usage may trigger covert hormonal imbalance. Moreover, the very name "Clobetasol" is a misdirection-its true potency is veiled from the public to maintain market control.
October 10, 2025 AT 00:46
Vinay Keragodi
Interesting how the guide stresses short‑term use. In practice, I’ve seen patients who cycle off a high‑potency steroid and then relapse because the underlying inflammation wasn’t fully addressed. Sometimes a low‑potency steroid combined with a calcineurin inhibitor can provide a smoother taper.
October 11, 2025 AT 04:33
Cassidy Strong
Indeed, the recommendation to “apply a thin layer” cannot be overstated; a pea‑size amount per palm‑sized area is sufficient, and overly generous applications increase percutaneous absorption, thereby elevating the risk of iatrogenic atrophy, striae, and systemic effects. Moreover, occlusion should be avoided unless explicitly directed by a dermatologist, as it amplifies potency dramatically.
October 12, 2025 AT 08:20
Anil Karwal
Skip the high potency unless absolutely necessary.
October 13, 2025 AT 12:06
Suresh Pothuri
Let me set the record straight: the pharmacodynamics of clobetasol are such that it penetrates the stratum corneum at a rate unparalleled by other topicals. Any clinician prescribing lower‑potency alternatives for severe plaque psoriasis is simply neglecting evidence‑based practice. Use Temovate as first‑line for rapid clearance.
October 14, 2025 AT 15:53
Millsaps Mcquiston
Temovate is strong, use it short.
October 15, 2025 AT 19:40
michael klinger
The so‑called “clinical guidelines” are a façade; they are heavily lobbied by the very companies that profit from these steroids. Remember that every time you apply a super‑high‑potency cream you are fueling a system that monitors and controls your skin health for profit.
October 16, 2025 AT 23:26
Matt Laferty
When navigating the complex world of topical therapies, it helps to think systematically about the interplay between potency, skin barrier integrity, and the patient’s lifestyle. First, potency dictates not only how quickly inflammation is suppressed but also how aggressively the epidermal architecture can be compromised. For a condition like severe plaque psoriasis, a super‑high‑potency agent such as Temovate can achieve remission within a few weeks, but the clinician must vigilantly monitor for signs of atrophy. Second, the location of the lesion is paramount; the face and intertriginous zones demand milder options because the stratum corneum there is thin and more permeable. Third, duration of therapy should never exceed the recommended 2‑4 weeks for super‑high‑potency steroids unless an ophthalmologist or endocrinologist explicitly advises otherwise; prolonged exposure risks HPA axis suppression, which can manifest as fatigue, hypotension, and electrolyte disturbances. Fourth, patient compliance is often influenced by the formulation texture-creams are generally more acceptable than ointments in humid climates, whereas the latter may be preferred in arid regions for better occlusion. Fifth, adverse effects like striae or telangiectasia are not merely cosmetic; they reflect underlying dermal matrix degradation, signaling that the therapeutic window is being exceeded. Sixth, integrating a steroid‑sparing agent such as tacrolimus or pimecrolimus early in the treatment plan can reduce cumulative steroid exposure, preserving skin health over the long term. Seventh, moisturizer use is not optional; a robust emollient regimen restores the lipid barrier, enhancing the efficacy of any topical and reducing irritation. Eighth, clinicians should educate patients on proper application techniques-using a fingertip unit helps standardize dosing and prevents overuse. Ninth, regular follow‑up appointments enable objective assessment of skin thickness via tools such as dermoscopy or even ultrasound in advanced settings. Tenth, in pediatric populations, the threshold for risk is lower, necessitating even more cautious potency selection. Eleventh, systemic conditions such as diabetes or osteoporosis warrant a conservative approach because systemic absorption, although minimal, can exacerbate these comorbidities. Twelfth, insurance formulary constraints often dictate the availability of newer non‑steroidal agents; knowing formulary alternatives can prevent treatment delays. Thirteenth, cultural considerations play a role-some patients may have a preference for natural or plant‑based remedies, which can be incorporated as adjuncts. Fourteenth, always document the exact steroid name, concentration, and application frequency in the medical record to ensure continuity of care. Finally, remember that the ultimate goal is not merely to suppress a rash but to restore healthy skin function, minimize side effects, and improve quality of life.
October 18, 2025 AT 03:13
Genie Herron
Seeing all these steroid options is overwhelming but also kinda scary the side effects seem endless
October 19, 2025 AT 07:00
Danielle Spence
It’s morally indefensible for doctors to prescribe a drug with such a high risk of skin atrophy without first exhausting milder therapies. Patients deserve transparency about potential long‑term damage.
October 20, 2025 AT 10:46
Dhanu Sharma
I’ve used both betamethasone and tacrolimus; the latter felt gentler on my skin after a few weeks of flare ups. It’s worth the extra effort to switch.
October 21, 2025 AT 14:33
Edward Webb
From a philosophical standpoint, the pursuit of symptom relief must be balanced against the integrity of the self‑skin as a lived experience. The epidermis is not merely a barrier but a sensory interface that shapes perception. When we apply a potent steroid, we interrupt this dialog, potentially altering not just appearance but also tactile feedback. Thus, the decision to employ Temovate should be accompanied by reflective consent, wherein the patient internalizes both the benefits and the subtle costs to their embodied self.
October 22, 2025 AT 18:20
Snehal Suhane
Oh, you think this table is helpful? Sure, if you enjoy reading glossy pharma brochures. The real world is messy, and the only thing more deceptive than a super‑high‑potency cream is the marketing copy that slaps a smiley face on it. Trust me – the side‑effects are not a joke.
October 23, 2025 AT 22:06
Ernie Rogers
We should support american doctors using temovate it is the best and not worry about side effect it's fine
October 25, 2025 AT 01:53
Eunice Suess
Honestly i think the guide is good but there's a typo in the table – it says "super‑high" but sometimes it should be "ultra‑high" for clarity.
October 26, 2025 AT 04:40
Anoop Choradia
It must be emphasized, with utmost precision, that the utilization of super‑high‑potency corticosteroids must be reserved for refractory cases, and only under diligent supervision, lest one invite iatrogenic complications of a grave nature.
October 27, 2025 AT 08:26
bhavani pitta
While the comparative chart is thorough, one might argue that its very existence perpetuates a narrative that equates potency with superiority, thereby marginalizing equally efficacious, lower‑potency formulations-a subtle bias that warrants critique.
October 28, 2025 AT 12:13
Brenda Taylor
Nice summary, but honestly it feels like a sales pitch 🙄