CPAP Pressure: How to Find the Right Setting for Better Sleep
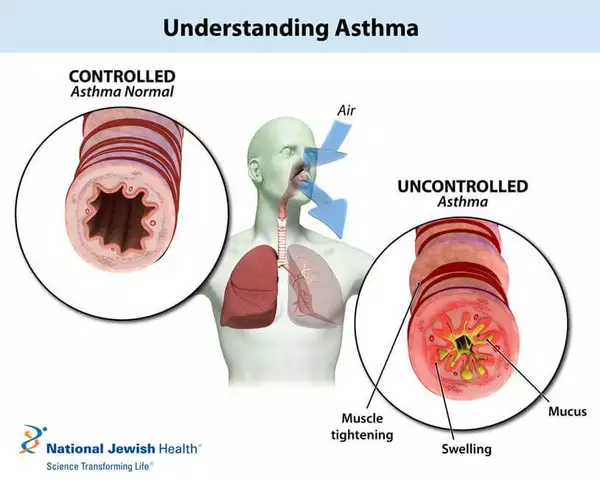
When you use a CPAP pressure, the continuous airflow level delivered by a sleep apnea machine to keep your airway open at night. It's not a one-size-fits-all number—it’s a personalized setting that can mean the difference between restful sleep and waking up exhausted. Too low, and your airway collapses. Too high, and you feel like you’re breathing through a straw. Many people never find their sweet spot because they assume the initial setting from their sleep study is final. But your needs change—weight, sleeping position, nasal congestion, even alcohol use—all shift what pressure works best.
CPAP machine settings, the adjustable airflow levels controlled by the device to treat obstructive sleep apnea aren’t just about numbers on a screen. They’re tied to your body’s real-time needs. For example, if you gain weight or start sleeping on your back more often, you might need higher pressure. If you lose weight or switch to side sleeping, you might need less. Some machines now auto-adjust pressure automatically, called APAP, which tracks your breathing and changes pressure throughout the night. But even those need occasional checks. And if you’re using a fixed-pressure CPAP, your doctor should review your data every 6–12 months. Most people don’t realize their machine stores detailed logs—how many apneas you had, how often you leaked air, how long you actually used it. That data is your roadmap to better sleep.
Sleep apnea treatment, the medical approach to managing breathing interruptions during sleep, often centered around CPAP therapy isn’t just about the machine. It’s about comfort. If your mask leaks, your pressure feels wrong, or your nose is dry, you’ll stop using it—and that’s the biggest failure in sleep apnea care. The right CPAP pressure should feel invisible. You shouldn’t notice it. If you do, something’s off. Try a different mask, use a humidifier, or ask about ramp settings that start low and slowly increase. Small tweaks make big differences. And if you’re still struggling, don’t assume it’s you. Talk to your provider. Maybe you need a different type of machine, or a BiPAP for higher pressure needs. Or maybe your sleep apnea has changed, and you need a new sleep study.
What you’ll find below are real stories and practical advice from people who’ve been there: how to tell if your pressure is too high or too low, how to read your machine’s data, what to ask your sleep doctor, and why some people need different pressure at night versus morning. These aren’t theory pieces—they’re fixes that worked. Whether you’re new to CPAP or have been using one for years, there’s something here that can help you breathe easier—literally.
Weight Loss and Sleep Apnea: How BMI Directly Impacts CPAP Pressure Needs
BMI directly affects how much pressure your CPAP machine needs to treat sleep apnea. Losing even 10% of your body weight can significantly reduce your AHI and lower CPAP pressure-sometimes eliminating the need for it entirely.