Antibiotic Selector Tool
Recommended Antibiotic for Your Situation
Full Comparison Table
| Antibiotic | Side Effects | Cost (10-day course) | Drug Interactions |
|---|
When you or a loved one need a prescription for a macrolide antibiotic, Clarithromycin is the active ingredient in the brand name Biaxin. Clarithromycin is a semi‑synthetic macrolide that works by blocking bacterial protein synthesis, making it effective against a broad range of gram‑positive and some gram‑negative organisms. It’s commonly prescribed for respiratory infections, skin infections, and certain atypical mycobacterial diseases.
Why Compare Biaxin with Other Options?
Patients often wonder whether another drug might be cheaper, have fewer side effects, or fit a specific infection better. Comparing Biaxin with its closest rivals - Azithromycin a once‑daily macrolide with a long half‑life, Erythromycin the older macrolide that can cause more gastrointestinal upset, Doxycycline a tetracycline useful for atypical pathogens, and Levofloxacin a fluoroquinolone with a broad spectrum but higher risk of tendon problems, gives you a clearer picture of what fits your health profile.
Quick Take
- Clarithromycin (Biaxin) offers strong activity against Respiratory infection pathogens and has a twice‑daily dosing schedule.
- Azithromycin is easier to take (once daily) but may be less potent for certain streptococcal infections.
- Erythromycin is cheap but notorious for stomach upset.
- Doxycycline works well for community‑acquired pneumonia and atypical bugs, but can cause photosensitivity.
- Levofloxacin covers a wider range of bacteria but carries a higher risk of tendon rupture and QT prolongation.
Decision Criteria: How to Pick the Right Antibiotic
Before you ask your doctor for a specific drug, think about these factors:
- Infection type - Some antibiotics are proven first‑line for certain conditions. For example, clarithromycin is a go‑to for Skin infection caused by *Staphylococcus aureus*, while doxycycline is preferred for *Chlamydia* pneumonia.
- Resistance patterns - Local antibiograms (lab‑generated resistance maps) may show rising macrolide resistance, nudging clinicians toward levofloxacin or combination therapy.
- Dosing convenience - Twice daily versus once daily can affect adherence, especially for children or busy adults.
- Side‑effect profile - If you have a history of GI upset, azithromycin may be gentler than erythromycin. If you’re prone to photosensitivity, avoid doxycycline on summer vacations.
- Drug interactions - Clarithromycin and erythromycin inhibit CYP3A4, which can bump up levels of statins, some anti‑arrhythmics, and certain anti‑seizure meds.
- Cost and insurance coverage - Generic doxycycline and erythromycin are usually cheaper than brand‑name Biaxin, but insurance formularies vary.
Side‑Effect Comparison
| Antibiotic | Typical GI issues | Key safety warning | Drug‑interaction risk |
|---|---|---|---|
| Clarithromycin (Biaxin) | Moderate nausea, abdominal pain | CYP3A4 inhibition → statin toxicity | High |
| Azithromycin | Mild diarrhea | QT prolongation in high doses | Medium |
| Erythromycin | Frequent heartburn, nausea | Hepatotoxicity rare | High |
| Doxycycline | Less GI upset, possible esophageal irritation | Photosensitivity, avoid pregnancy | Low |
| Levofloxacin | Occasional nausea | Tendon rupture, QT prolongation | Medium |
Cost Snapshot (U.S. average retail, 2025)
- Clarithromycin (brand Biaxin): $75‑$120 for a 10‑day course.
- Azithromycin (generic): $15‑$30 for a 5‑day pack.
- Erythromycin (generic): $10‑$20 for a 10‑day pack.
- Doxycycline (generic): $8‑$15 for a 10‑day pack.
- Levofloxacin (generic): $25‑$45 for a 7‑day pack.
Insurance formularies often place macrolides at Tier2, while doxycycline is usually Tier1. Always check your plan’s current pricing before committing.
Best‑Fit Scenarios
Here’s a quick guide on which antibiotic shines for common infections:
| Infection | Top Choice | Why |
|---|---|---|
| Community‑acquired pneumonia | Clarithromycin | Strong activity against atypical *Mycoplasma* and *Legionella*. |
| Sinusitis (bacterial) | Azithromycin | Once‑daily dosing improves adherence. |
| Skin and soft‑tissue infection | Doxycycline | Covers MRSA and atypical organisms without GI upset. |
| Travel‑related diarrhea | Erythromycin | Effective against *Campylobacter* and cheap. |
| Complicated urinary tract infection | Levofloxacin | Broad spectrum and good tissue penetration. |
How to Talk to Your Doctor
Armed with this comparison, you can ask focused questions:
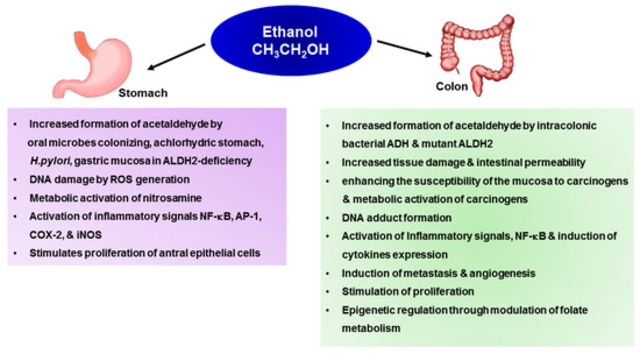
- “Given my recent *H. pylori* history, is clarithromycin still safe, or should we consider doxycycline?”
- “If I’m on a statin, can we avoid clarithromycin to prevent muscle toxicity?”
- “What’s the cheapest effective option for a 7‑day sinus infection?”
Doctors appreciate when you bring specific concerns; it speeds up the decision process and improves adherence.
Potential Pitfalls to Avoid
Even the best‑matched antibiotic can backfire if used incorrectly. Keep these warnings in mind:
- Never stop a course early because you feel better - resistance can develop.
- Take macrolides with food if you experience stomach upset, but avoid grapefruit juice (CYP3A4 interaction).
- If you develop a rash or severe diarrhea, seek medical help right away; it could signal a *Clostridioides difficile* infection.
- Women who are pregnant should avoid doxycycline due to potential tooth discoloration in the fetus.
Frequently Asked Questions
Is Biaxin more effective than azithromycin for pneumonia?
Clarithromycin generally provides broader coverage against atypical organisms like *Mycoplasma pneumoniae* and *Legionella pneumophila*. If local resistance to macrolides is low, Biaxin is often preferred, but azithromycin remains a viable once‑daily alternative when dosing convenience is key.
Can I take clarithromycin with a cholesterol‑lowering statin?
Because clarithromycin inhibits CYP3A4, it can raise blood levels of statins like simvastatin and atorvastatin, increasing the risk of muscle damage. Ask your doctor to switch to a statin that’s less dependent on CYP3A4 (e.g., pravastatin) or to use an alternative antibiotic.
What should I do if I develop a rash while on Biaxin?
Stop the medication immediately and contact your healthcare provider. A rash can signal a hypersensitivity reaction, and you may need a different class of antibiotic.
Is doxycycline safe for children?
Doxycycline is usually avoided in children under 8years because it can cause permanent tooth discoloration. In emergencies, the benefits may outweigh the risk, but alternatives like azithromycin are preferred.
Why does clarithromycin sometimes cause a metallic taste?
The metallic sensation is a known, mild side effect of many macrolides, stemming from their impact on taste buds and saliva composition. It usually fades after a few days of therapy.
Can I use levofloxacin if I have a tendon injury?
Fluoroquinolones like levofloxacin have been linked to tendon rupture, especially in people over60or those on steroids. Discuss alternative antibiotics with your doctor if you have a tendon problem.
Choosing the right antibiotic is a balance of infection type, side‑effect tolerance, drug interactions, and cost. With this side‑by‑side view of Biaxin and its main competitors, you can have a more informed conversation with your prescriber and land on the safest, most effective option for your situation.







October 2, 2025 AT 12:26
Emily Stangel
When evaluating macrolide therapy, it is essential to adopt a systematic framework that integrates pharmacodynamic potency, patient-specific risk factors, and health‑economic considerations. Clarithromycin, marketed as Biaxin, exhibits a robust spectrum against atypical respiratory pathogens, which justifies its frequent recommendation in community‑acquired pneumonia guidelines. Nevertheless, the drug’s propensity for CYP3A4 inhibition imposes a non‑trivial interaction burden with statins, certain anti‑arrhythmics, and immunosuppressants. The clinical relevance of such interactions is amplified in polypharmacy contexts, particularly among elderly patients with multimorbidity. In parallel, the gastrointestinal adverse‑effect profile of clarithromycin-moderate nausea and abdominal discomfort-must be weighed against the comparatively milder diarrheal tendencies of azithromycin. Cost analysis further complicates decision making, as the retail price of a ten‑day Biaxin course significantly exceeds that of generic alternatives such as doxycycline or erythromycin. Insurance formularies often mitigate this disparity through tiered copayment structures, yet out‑of‑pocket expenses remain a decisive factor for many individuals. From an adherence perspective, the twice‑daily dosing schedule of clarithromycin may pose challenges for patients with erratic daily routines, whereas azithromycin’s once‑daily regimen enhances convenience. Moreover, emerging resistance patterns in certain geographic regions have prompted caution in the indiscriminate use of macrolides, encouraging clinicians to consult local antibiograms before finalising therapy. While levofloxacin provides a broad‑spectrum option with convenient dosing, its association with tendon rupture and QT prolongation necessitates careful patient selection. In summary, the optimal antibiotic choice emerges from a balanced appraisal of infection site, microbial susceptibility, drug‑interaction risk, side‑effect tolerability, dosing convenience, and economic impact. Clinicians are advised to engage patients in shared decision‑making, ensuring that the selected regimen aligns with both therapeutic goals and individual preferences. Ultimately, a nuanced, patient‑centred approach supersedes simplistic drug‑centric algorithms. Future research should continue to elucidate comparative effectiveness in diverse patient populations. Such evidence will further refine antimicrobial stewardship initiatives.
October 3, 2025 AT 07:53
Suzi Dronzek
It is astonishing how often patients are steered toward clarithromycin without a sober assessment of its drawbacks. The author’s attempt to glorify Biaxin betrays a naive optimism that disregards the severe drug‑interaction hazards inherent to macrolides. One cannot ignore that CYP3A4 inhibition can precipitate life‑threatening statin toxicity, a fact that is glossed over in the glossy overview. Moreover, the claim of “strong activity” against atypical pathogens is an oversimplification; regional resistance data reveal an unsettling upward trend in macrolide‑resistant strains. The cost argument presented is equally myopic, focusing solely on retail price while omitting the hidden expenses of managing adverse events. A thorough analysis would also consider patient adherence, yet the twice‑daily regimen of clarithromycin is presented without critique, despite evidence that it reduces compliance in busy populations. The comparison table omits a crucial column for contraindications, which renders the evaluation incomplete. Finally, the piece fails to address alternative first‑line agents that boast superior safety profiles and comparable efficacy. In short, the article reflects a partial narrative that risks misinforming readers and perpetuating suboptimal prescribing patterns.
October 4, 2025 AT 03:20
Aakash Jadhav
Yo, reading that chart felt like watching a soap opera where the heroes keep swapping costumes every other episode.
Clarithromycin strutted in like the charismatic lead, but then Azithromycin swooped in with a one‑day cameo that stole the spotlight.
The drama peaks when Erythromycin shows up, causing stomach turmoil like an angry plot twist.
Meanwhile Doxycycline drops a side‑effect bomb of photosensitivity that makes you think the sun’s out to get you.
Levofloxacin tries to be the dark anti‑hero, whispering promises of broad coverage while warning about tendon drama.
Honestly, the whole showdown is a reminder that picking an antibiotic is like casting for a blockbuster – you need the right star for the right scene.
Just don’t forget the supporting cast of drug interactions, they’re the real plot‑twisters.
In the end, the audience (that’s us) decides which performance gets the standing ovation.
October 4, 2025 AT 22:46
Amanda Seech
I think the post does a good job but i have a few thigns to add.
i try to keep medicaion simple so i like doxy when i can becasue it's cheap and has less tummy upset.
if you have a sore stomach clarithro might be rough.
also watch out for statin mix if you take them.
October 5, 2025 AT 18:13
Lisa Collie
One must interrogate the intellectual rigor underpinning the author’s selection hierarchy. The insinuation that clarithromycin reigns supreme betrays a constricted epistemic lens that neglects the nuanced pharmacoeconomic tableau. By privileging a brand‑name entity, the narrative tacitly reinforces pharmaceutical hegemony, a point seldom illuminated in such expositions. Moreover, the cursory treatment of drug‑interaction matrices reflects an alarming paucity of scholarly depth. An erudite discourse would juxtapose pharmacokinetic subtleties across all agents, rather than capitulating to a facile cost‑benefit equation. In light of these considerations, the article appears as a perfunctory advertisement masquerading as clinical guidance.
October 6, 2025 AT 13:40
Avinash Sinha
Behold the kaleidoscopic tapestry of antimicrobial choices, each hue shimmering with its own therapeutic promise! Clarithromycin swirls in regal indigo, promising a royal siege on atypical marauders, yet its undertow of CYP3A4 turbulence can capsize even the sturdiest statin‑laden vessel. Azithromycin pirouettes in sunlit gold, a single‑daily pirouette that waltzes through compliance hurdles, though its modest potency sometimes leaves the battlefield seeking reinforcements. Erythromycin drapes itself in earthy amber, cheap yet notorious for conjuring fiery gastric comets that can eclipse patient comfort. Doxycycline blossoms in verdant green, flaunting MRSA mastery while sprinkling photosensitivity pixie‑dust upon sun‑kissed skin. Levofloxacin, the tempestuous crimson, storms through a broad spectrum but threatens tendon rupture with a spear of peril. In this vibrant tableau, the prescriber must wield a discerning brush, painting a regimen that marries efficacy, safety, and the patient’s lived canvas.
October 7, 2025 AT 09:06
ADAMA ZAMPOU
From a philosophical standpoint, the selection of an antibiotic can be likened to the age‑old dialectic between necessity and virtue. While clarithromycin offers undeniable pharmacological potency, it simultaneously imposes a moral responsibility upon the clinician to weigh its interaction potential against the sanctity of patient wellbeing. In the grand schema of therapeutic decision‑making, one must consider not only the immediate eradication of pathogenic entities but also the long‑term repercussions on microbiological equilibrium. Hence, the discourse transcends mere cost analysis, inviting a deeper contemplation of stewardship, the ethical stewardship of antimicrobial resources, and the societal covenant to preserve efficacy for future generations.
October 8, 2025 AT 04:33
Liam McDonald
I understand the concerns regarding CYP3A4 inhibition however the benefits can outweigh the risks when applied judiciously. Patients with severe atypical pneumonia often experience rapid resolution with clarithromycin and that clinical gain should not be dismissed outright. It is also worth noting that many insurance plans now provide tiered coverage that lessens the financial burden for many. In practice a thorough medication reconciliation can mitigate most interaction hazards. Ultimately shared decision making remains the cornerstone of responsible prescribing.
October 9, 2025 AT 00:00
Adam Khan
The article suffers from a litany of syntactic oversights that undermine its credibility. For instance, the phrase "once‑daily dosing improves adherence" lacks a definitive article and should read "a once‑daily dosing regimen improves adherence". Moreover, the inconsistent use of the Oxford comma throughout the list of side‑effects creates ambiguity. From a terminological perspective, the term "broad spectrum" is employed without qualifier, rendering the statement scientifically vague. A rigorous editorial process would rectify these lapses, thereby reinforcing the article’s authority in the clinical discourse.
October 9, 2025 AT 19:26
rishabh ostwal
It is incumbent upon us to adhere to a principled hierarchy when prescribing, lest we succumb to the allure of convenience at the expense of patient safety. While the author extols the virtues of clarithromycin, one must recall the moral imperative to avoid exposing patients to heightened QT prolongation risks when alternative agents suffice. The ethical calculus demands that we prioritize agents with lower interaction profiles, especially for individuals already burdened with polypharmacy. The discourse would benefit from a more stringent moral lens, ensuring that therapeutic enthusiasm does not eclipse prudential restraint.
October 10, 2025 AT 14:53
Allison Metzner
What the pharmaceutical conglomerates don’t want you to realize is that the data presented here is cherry‑picked to push a market‑dominant brand while obscuring the lurking specter of resistance. The subtle narrative nudges prescribers toward Biaxin, subtly reinforcing a profit‑driven agenda that eclipses genuine patient‑centred care. By omitting the long‑term ecological impact on microbiota and the insidious rise of macrolide‑resistant organisms, the piece becomes a vehicle for covert manipulation. We must interrogate these hidden motives and demand transparent, unbiased evidence before accepting such recommendations.
October 11, 2025 AT 10:20
Kay Yang
Interesting perspective 😊 It’s helpful to see the trade‑offs laid out so clearly, especially when navigating insurance formularies and patient preferences.
October 12, 2025 AT 05:46
william smith
In practice, start with clarithromycin for atypical pneumonia, and switch to a safer alternative if side effects become problematic.
October 13, 2025 AT 01:13
Timothy Javins
Nevertheless, cost considerations often dominate prescribing habits.