Every year, millions of Americans skip doses, split pills, or skip refills altogether because they can’t afford their prescriptions. It’s not laziness. It’s not ignorance. It’s simple math: a $400 monthly pill doesn’t fit into a $2,000 monthly budget after rent, food, and utilities. But here’s the truth most people don’t know - there’s often a cheaper version that works just as well. Not a generic. Not a coupon. A different medication entirely, from the same class, with the same effect, but at a fraction of the price. This is called a therapeutic alternative, and asking for one could save you hundreds - even thousands - a year.
What Is a Therapeutic Alternative?
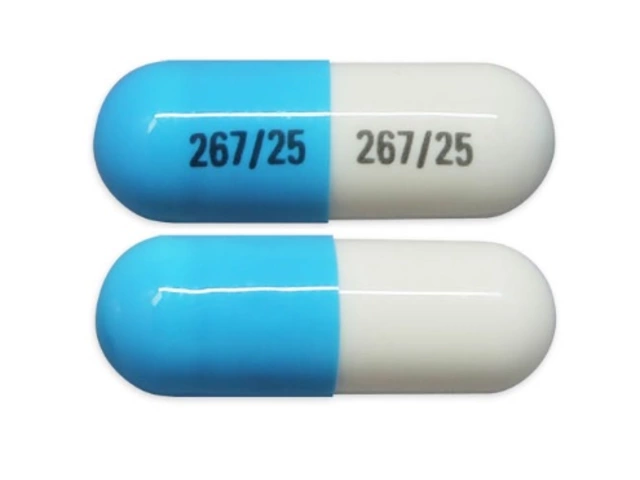
A therapeutic alternative isn’t the same as a generic. Generics are exact copies of brand-name drugs - same active ingredient, same dose, same shape. A therapeutic alternative is a different drug altogether, but one that treats the same condition in a similar way. For example:- Instead of esomeprazole (Nexium), you could take omeprazole - same heartburn relief, 96% cheaper.
- Instead of Lyrica (pregabalin), you could try gabapentin - same nerve pain control, 97% cheaper.
- Instead of Eliquis (apixaban), you could use warfarin - same blood thinner, 90% cheaper.
These aren’t experimental swaps. They’re backed by clinical trials, approved by the FDA, and used daily in hospitals and clinics. The difference? One costs $30 a month. The other costs $450. And yet, many doctors never mention them unless you ask.
Why Don’t Doctors Always Suggest Cheaper Options?
It’s not that they don’t care. It’s that they’re overwhelmed. Most primary care doctors see 25-30 patients a day. Each visit lasts 10-15 minutes. They’re juggling charts, insurance forms, and electronic alerts. Asking about cost isn’t always part of the routine.Plus, some providers worry that switching meds might cause problems. They’ve seen patients react differently to similar drugs - one person’s miracle drug is another person’s side effect nightmare. That’s valid. But the fear of change shouldn’t block the chance to save money - especially when the evidence supports the swap.
A 2023 survey by the American Academy of Family Physicians found that 43% of patients said their doctor was hesitant to consider cheaper alternatives. That’s not because doctors are against savings. It’s because they’re not trained to lead the conversation. You have to bring it up.
How to Ask for a Lower-Cost Alternative
You don’t need to be a medical expert. You just need to be clear, prepared, and polite. Here’s how to do it in five steps:- Start with cost. Say it outright: “I’m having trouble affording my prescription. Is there a cheaper option that works just as well?” This is the exact phrase recommended by the AAFP. It’s simple, non-confrontational, and opens the door.
- Do your homework. Before your appointment, check GoodRx or your pharmacy’s $4 list. Look up your drug. See what alternatives exist. For example, if you’re on atorvastatin (Lipitor), you might find that rosuvastatin (Crestor) is more expensive - but simvastatin is on the $4 list. Bring that info with you.
- Ask for specifics. Don’t just say, “Is there something cheaper?” Say, “Could I try omeprazole instead of esomeprazole? I saw it’s the same class and costs $15 a month.” Specificity makes it easier for your doctor to say yes.
- Ask about coverage. Some alternatives require prior authorization. Ask: “Will my insurance cover this? Do I need a form filled out?”
- Follow up. If your doctor says no, ask why. Is it because of side effects? Efficacy? Or just habit? If they’re unsure, suggest a trial. “Can we try it for 30 days and see how I feel?”

Where to Find Therapeutic Alternatives
You don’t have to guess. There are trusted, free tools to help you find cheaper options:- GoodRx - Enter your drug. It shows prices at nearby pharmacies and lists therapeutic alternatives with side-by-side cost comparisons. It covers over 6,000 medications.
- Walmart, CVS, Walgreens $4 Lists - These pharmacies offer 30-day supplies of common meds like metformin, lisinopril, and atorvastatin for $4. No insurance needed.
- NeedyMeds.org - Lists patient assistance programs from drug manufacturers. Many offer free or $0 copay meds for those under 400% of the federal poverty level.
- RxAssist.org - A nonprofit database of free and low-cost programs for prescription drugs.
One patient in Ohio switched from Jardiance ($500/month) to metformin ($12/month) and saved $5,856 a year. Another in Texas replaced Humira with a biosimilar after their doctor approved it - cutting their bill from $6,000 to $800.
When It Won’t Work
Therapeutic alternatives aren’t magic. Some drugs have no equivalent. This is especially true for:- Biologics (like Humira, Enbrel, Ocrevus)
- Specialty cancer drugs
- Some rare disease treatments
According to the Congressional Budget Office, about 15% of drug classes have no viable therapeutic alternatives. In those cases, your best bet is manufacturer coupons, patient assistance programs, or applying for Medicaid.
Also, not every patient responds the same. A 2021 study in JAMA Internal Medicine found that 8-12% of people with diabetes had different blood sugar results when switching between GLP-1 agonists. That’s why you never switch without medical supervision. But that’s also why you should ask - and then monitor how you feel.
What to Do If Your Doctor Says No
If your doctor refuses, don’t give up. Ask for a reason. If they say, “It’s not as effective,” ask for the evidence. If they say, “I’ve never seen it work,” ask if they’ve tried it with other patients.You can also request a tiering exception with your insurance. If your drug is on a high tier (meaning high copay), you can ask your insurer to move you to a lower tier if a cheaper alternative is clinically appropriate. Medicare Part D requires insurers to respond to these requests within 72 hours for urgent cases.
Some patients have had success by asking for a second opinion - especially from a pharmacist. Many pharmacies now offer free medication reviews. Bring your list of drugs, your symptoms, and your budget. Pharmacists are trained to spot therapeutic alternatives and often know more about cost than doctors do.
Real Results: What People Are Saving
GoodRx’s 2024 survey of 12,500 patients found that 68% successfully got a cheaper alternative through their doctor. The average monthly savings? $47.25. That’s $567 a year. Multiply that by five meds? That’s over $2,800.Here are real examples from patients:
- Switched from Eliquis to warfarin - saved $450/month.
- Switched from Lyrica to gabapentin - saved $435/month.
- Switched from Creon (pancreatic enzyme) to a generic equivalent - saved $220/month.
- Switched from Trulicity to metformin - saved $400/month.
One woman in Florida told Healthgrades she was skipping her Xarelto doses 40% of the time because of cost. After switching to warfarin, she took every pill - and avoided a stroke.
What’s Changing in 2025
New tools are making therapeutic alternatives easier to access. In October 2024, Medicare updated its rules to require all Part D plans to use the same criteria for approving cost-saving swaps. In January 2025, Epic and Cerner - the two biggest electronic health record systems - added new prompts that suggest alternatives at the moment the doctor is writing the prescription.AI tools are also being tested. A 2024 study showed an AI system identified 89% of correct therapeutic swaps - better than human doctors at 72%. That means in the near future, your doctor’s computer might suggest a cheaper option before they even finish typing.
And while the Inflation Reduction Act lets Medicare negotiate prices for some high-cost drugs, experts say therapeutic interchange will still be essential. Why? Because even after negotiation, a $300 drug might still be twice as expensive as a $150 alternative that works just as well.
Final Thought: You Have Power
Prescription costs aren’t just a pharmacy problem. They’re a patient problem. And you’re not powerless. You have the right to ask. You have the right to know. And you have the right to try something cheaper - as long as it’s safe.Next time you get a prescription, don’t just take it. Ask: “Is there a version that costs less - and still works?” It could change your budget. It could change your health. And it might just save your life.
Can I switch to a cheaper medication without my doctor’s approval?
No. Never switch or stop a prescribed medication without talking to your doctor. Even if a drug looks like a cheaper version, it may have different dosing, side effects, or interactions. Therapeutic alternatives require clinical judgment. Your doctor can help you make a safe switch - and monitor your response.
Are therapeutic alternatives as effective as brand-name drugs?
Yes - when chosen correctly. Many therapeutic alternatives have been tested in head-to-head clinical trials and shown to be equally effective. For example, omeprazole and esomeprazole have nearly identical outcomes for acid reflux. The key is matching the drug to your condition, not just the price. Always follow up with your doctor after switching.
What if my insurance won’t cover the cheaper option?
Ask for a tiering exception. Your doctor can submit a form explaining why the cheaper alternative is medically appropriate. Medicare and most private insurers must respond within 72 hours for urgent cases. If denied, you can appeal. Many patients succeed on the second try - especially with documentation from their provider.
Can I use GoodRx with my insurance?
Sometimes. GoodRx shows you the cash price at pharmacies - which is often lower than your insurance copay. If the GoodRx price is cheaper, you can choose to pay cash instead of using insurance. Just ask the pharmacist to process it as a cash transaction. This works best for generics and therapeutic alternatives on the $4 list.
How do I know if a therapeutic alternative is right for me?
Ask your doctor three questions: 1) Is this alternative proven to work for my condition? 2) Are the side effects similar? 3) Will I need to adjust my dose or monitor anything differently? If the answer to all three is yes, it’s likely a good fit. Start with a 30-day trial and track how you feel - then follow up.
Therapeutic alternatives aren’t a loophole. They’re a standard part of medical practice - used in hospitals, taught in med school, and backed by decades of research. The only thing missing is you asking for it.