Glucophage Trio vs Alternatives: Treatment Selector
Select Your Key Priorities
Answer these questions to find the best treatment option for your situation.
Recommended Treatment Based on Your Profile
Quick Takeaways
- Glucophage Trio combines three mechanisms in one pill, which can simplify dosing but may limit dose flexibility.
- Alternatives such as SGLT2 inhibitors or GLP‑1 agonists often provide greater cardiovascular benefit.
- Side‑effect profiles differ: sulfonylureas risk hypoglycemia, while metformin can cause GI upset.
- Cost varies widely; generics of individual components are cheap, but brand‑only combinations can be pricey.
- Choosing the right regimen depends on kidney function, weight goals, and cardiovascular risk.
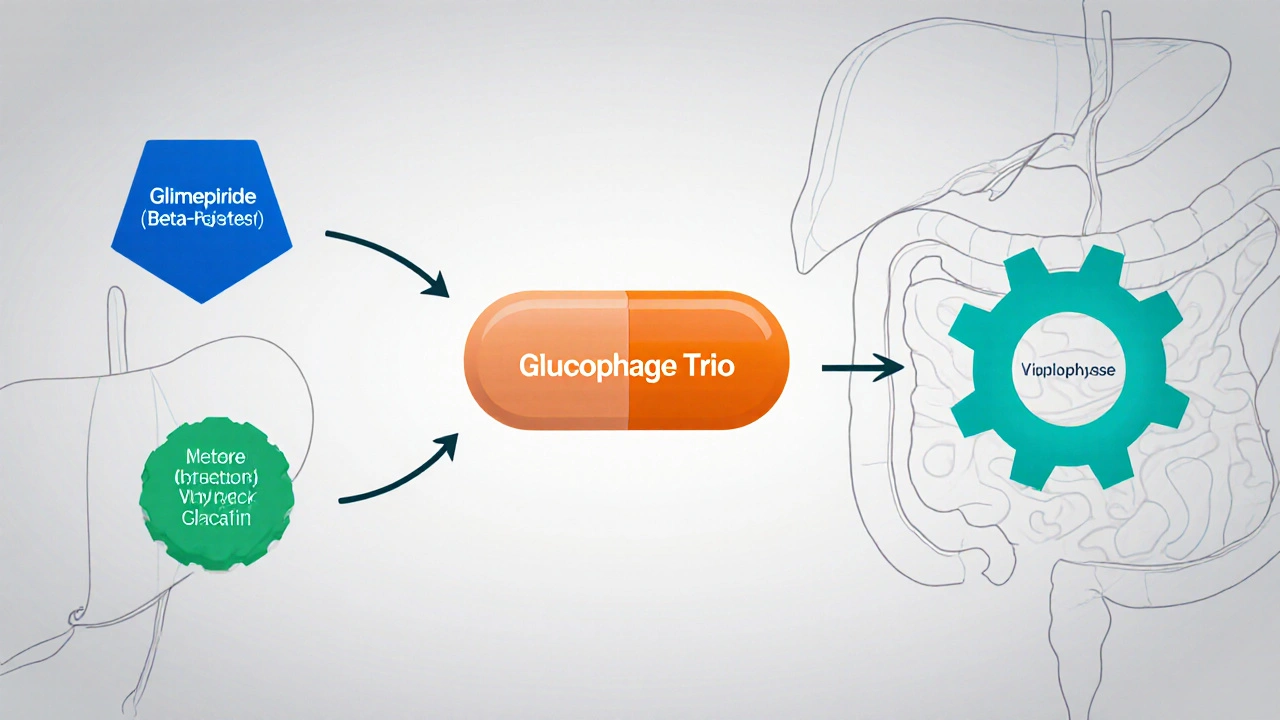
What is Glucophage Trio?
When treating type2 diabetes, Glucophage Trio is a fixed‑dose combination that packs glimepiride, metformin, and voglibose into one tablet. The idea is to hit three different pathways at once: boost insulin release, suppress liver glucose output, and slow carbohydrate absorption.
The three pieces of the puzzle
Glimepiride belongs to the sulfonylurea class. It binds to pancreatic beta‑cell receptors, prompting a surge of insulin. This works fast, but the trade‑off is a higher chance of low blood sugar, especially if meals are missed.
Metformin is a biguanide and the most prescribed first‑line drug worldwide. It mainly cuts the liver’s gluconeogenesis and improves peripheral insulin sensitivity. Most patients tolerate it well, though up to 30% report mild nausea or diarrhea initially.
Voglibose is an alpha‑glucosidase inhibitor. By blocking the brush‑border enzymes that break down starch, it blunts post‑meal glucose spikes. Its effect is modest, but it can smooth out the peaks that cause oxidative stress.
Benefits and drawbacks of the combo
Putting all three agents together means fewer pills-great for people who struggle with complex regimens. In clinical practice, the average HbA1c reduction observed with Glucophage Trio is about 1.5% after three months, comparable to many dual‑therapy strategies.
However, the fixed ratio limits dose tweaking. If a patient needs more metformin but tolerates only a low dose of glimepiride, the combo forces a compromise or a switch back to separate tablets. Also, the side‑effect profiles stack: gastrointestinal upset from metformin, hypoglycemia risk from glimepiride, and possible flatulence from voglibose.
Cost is a mixed bag. Generic versions of the three components are cheap, but the branded combination often carries a premium, especially in the United States where insurance formularies may prefer separate generics.
Alternative oral and injectable options
Most clinicians consider several other drug classes when Glucophage Trio isn’t the best fit. Here’s a quick snapshot of the most common alternatives:
- Pioglitazone - a thiazolidinedione that improves insulin sensitivity in muscle and fat.
- Sitagliptin - a DPP‑4 inhibitor that raises incretin levels, enhancing glucose‑dependent insulin release.
- Empagliflozin - an SGLT2 inhibitor that forces excess glucose out through the urine, also lowering blood pressure and offering heart‑failure protection.
- Liraglutide - a GLP‑1 receptor agonist injected once daily, known for weight loss and strong cardiovascular benefit.
Side‑effect and safety snapshot
Each alternative brings its own safety considerations:
- Pioglitazone can cause fluid retention and is contraindicated in heart‑failure patients.
- Sitagliptin is generally well‑tolerated, but rare cases of pancreatitis have been reported.
- Empagliflozin may trigger genital yeast infections and, in rare cases, diabetic ketoacidosis.
- Liraglutide often leads to nausea, but the weight‑loss effect can be a major plus for obese patients.
Head‑to‑head comparison
| Drug (or combo) | Primary Mechanism | Typical HbA1c Drop | Key Side‑effects | Cardiovascular Benefit | Average Monthly Cost (US$) |
|---|---|---|---|---|---|
| Glucophage Trio | Sulfonylurea+Biguanide+Alpha‑glucosidase inhibitor | ~1.5% | Hypoglycemia, GI upset, flatulence | Neutral | ≈$85 (brand) |
| Pioglitazone | Thiazolidinedione - insulin sensitizer | ~0.8% | Weight gain, edema, heart‑failure risk | Neutral | ≈$30 (generic) |
| Sitagliptin | DPP‑4 inhibitor - incretin enhancer | ~0.7% | Headache, rare pancreatitis | Neutral | ≈$250 (brand) |
| Empagliflozin | SGLT2 inhibitor - urinary glucose excretion | ~0.9% | UTI, genital mycotic infections, DKA | Reduced CV death & HF hospitalization | ≈$300 (brand) |
| Liraglutide | GLP‑1 receptor agonist - glucose‑dependent insulin release | ~1.2% | Nausea, vomiting, rare pancreatitis | Significant CV benefit, weight loss | ≈$450 (brand) |
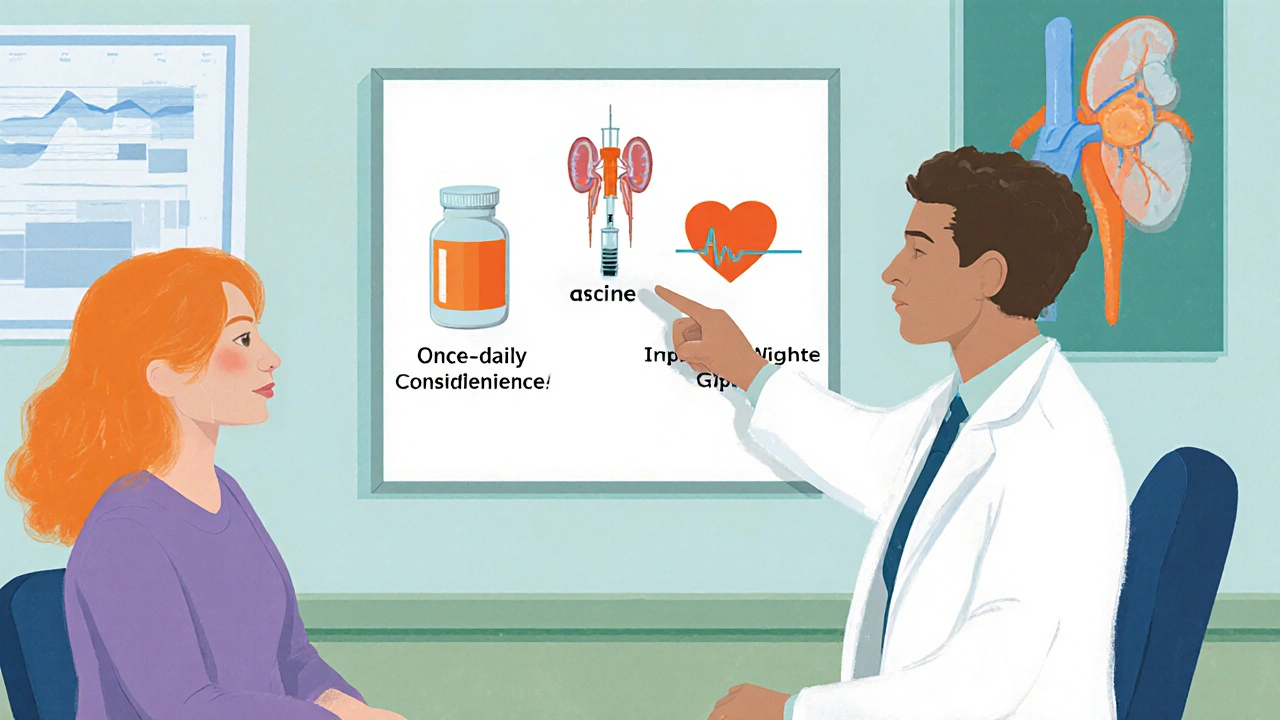
How to decide which regimen fits you
Think of medication choice as a match‑making exercise. Ask yourself these three questions:
- Do I need a simple once‑daily pill, or can I handle injections?
- Is weight loss a priority, or am I okay with a neutral effect?
- Do I have heart‑failure, chronic kidney disease, or a history of hypoglycemia?
If you answered “yes” to #1 and “no” to #2 and #3, GlucophageTrio’s convenience might win. If cardiovascular protection or weight loss matters, an SGLT2 inhibitor or GLP‑1 agonist usually edges out the combo.
Kidney function is a hard limit. Metformin’s dose must be reduced when eGFR <45mL/min/1.73m², and SGLT2 inhibitors lose efficacy below 30. Sulfonylureas can be used down to 15, but the hypoglycemia risk climbs.
Practical tips for switching or starting therapy
- Start low, go slow: If moving from separate tablets to Glucophage Trio, begin with the lowest dose and monitor blood sugar for two weeks.
- Check renal function before any metformin‑based regimen; adjust dose or choose an alternative if eGFR <30.
- When adding an SGLT2 inhibitor, ensure patients are educated about hydration and genital infection signs.
- For injectables like liraglutide, arrange training on pen use and emphasize gradual dose escalation to avoid nausea.
- Review insurance formularies early; some plans require prior authorization for newer agents.
Frequently Asked Questions
Can I take Glucophage Trio if I have kidney disease?
Metformin, a key part of the trio, needs dose reduction when eGFR falls below 45mL/min/1.73m² and should be stopped under 30. If your kidney function is borderline, your doctor may keep you on a lower‑dose metformin-only regimen and add another class instead.
Do I need to worry about hypoglycemia with Glucophage Trio?
Yes, the glimepiride component can cause low blood sugar, especially if meals are skipped or alcohol is consumed. Monitoring glucose before bedtime and having a fast‑acting carbohydrate on hand are good safety habits.
How does the efficacy of Glucophage Trio compare to a GLP‑1 agonist?
In head‑to‑head trials, liraglutide typically lowers HbA1c by about 1.2% and also promotes 3‑5kg of weight loss. Glucophage Trio reduces HbA1c by roughly 1.5% but has a neutral effect on weight and carries a hypoglycemia risk. If weight loss and cardiovascular protection matter, the GLP‑1 option often wins.
Is the combo cheaper than buying the three pills separately?
For patients with generic coverage, the three separate tablets usually cost less-around $30‑$45 per month. The branded Glucophage Trio can run $80‑$100, though some insurance plans offer discounts that narrow the gap.
Can I combine Glucophage Trio with other diabetes drugs?
Yes, many clinicians add an SGLT2 inhibitor or a GLP‑1 agonist on top of the trio for extra control and cardiovascular benefit. However, avoid stacking another sulfonylurea or a high‑dose insulin without close monitoring.







October 4, 2025 AT 15:54
Roxanne Porter
Thank you for the thorough overview of Glucophage Trio and its alternatives. The structured comparison table is particularly helpful for clinicians who need to make quick decisions. I appreciate the clear delineation of cardiovascular benefits across the drug classes. It is also useful to see the cost considerations presented side by side. Overall, this guide serves as a solid reference for both patients and healthcare providers.
October 5, 2025 AT 19:41
Jonathan Mbulakey
Interesting read, especially the way the article splits the decision‑making into three simple questions. It feels a bit like philosophical Zen – ask the right questions and the path becomes clear. The balance between convenience and efficacy is well‑captured. I’m leaning toward the combo for its pill simplicity, though the injection options have their own charm.
October 6, 2025 AT 23:27
Warren Neufeld
This breakdown makes it easier to understand what each drug does. The side‑effect list is simple and straight to the point. It’s good to see that metformin’s GI upset is mentioned, as many patients worry about that. I think the article does a nice job helping people match their health goals with the right medication.
October 8, 2025 AT 03:14
Deborah Escobedo
Great summary, very clear and encouraging!
October 9, 2025 AT 07:01
Dipankar Kumar Mitra
Look, the combo sounds neat until you realize you’re stuck with a fixed ratio. If a patient needs more metformin but less sulfonylurea, you’re forced into a compromise. The side‑effects stack like a bad pizza topping – GI upset, hypoglycemia, flatulence. In real life, flexibility matters more than convenience.
October 10, 2025 AT 10:47
Tracy Daniels
Nice detailed table! It really helps to compare costs and benefits side‑by‑side. The clear headings make it easy to skim. 😊 Keep up the good work!
October 11, 2025 AT 14:34
Hoyt Dawes
Ah, the drama of modern pharmacotherapy! One cannot simply parade a three‑in‑one pill without acknowledging its theatrical shortcomings. First, the fixed‑dose design is a rigid script that offers no improvisation for dose titration. Imagine a patient craving more metformin; the script forces a cruel compromise, leaving the sulfonylurea lingering like an unwanted understudy. Second, the side‑effect ensemble-hypoglycemia, gastrointestinal turmoil, and that dreaded flatulence-perform in unison, creating a cacophony of discomfort. The audience, i.e., the patient, is left bewildered, clutching at the hope of a simpler regimen. Third, the cost narrative is a tragic tale; while generic components are cheap, the branded combination charges a premium worthy of a Broadway production. This financial burden often alienates the very patients it aims to serve. Moreover, the cardiovascular neutrality of Glucophage Trio is a stark contrast to the heroic acts of SGLT2 inhibitors and GLP‑1 agonists, which stride onto the stage with proven heart‑failure benefits. In the grand theater of diabetes management, the combo merely plays a supporting role, never the lead. Let us not be fooled by the allure of convenience; medicine demands nuance, not a one‑size‑fits‑all monologue. The true art lies in tailoring therapy to individual physiology, not shoving all actors into a single, cramped scene. Therefore, clinicians must weigh the melodrama of side‑effects, cost, and lack of cardiovascular impact against the fleeting applause of pill simplicity. In my view, the script should be rewritten, allowing flexibility, safety, and efficacy to take center stage.
October 12, 2025 AT 18:21
Jeff Ceo
Your point about flexibility is spot on. Patients need the ability to adjust doses without compromising safety. I’d add that renal function should always be the gatekeeper before prescribing metformin‑based combos. Thanks for the concise reminder.
October 13, 2025 AT 22:07
David Bui
Dipankar makes a good point about fixed ratios but the article already says that you cant tweak doses if you need more metformin you’re stuck the combo is just a convenience pill it isn’t a miracle drug
October 15, 2025 AT 01:54
Alex V
Ah, the wonderful world of “expert” commentary-how reassuring to see yet another self‑appointed guru spewing sarcasm like confetti at a parade. Let’s dissect this with the rigor of a conspiracy theorist hunting for hidden agendas. First, the obvious: the article is a corporate‑sponsored sales pitch masquerading as unbiased education, designed to push a pricey brand combo into the hands of unsuspecting patients. Second, the so‑called “cardiovascular neutrality” is a convenient lie, because the pharma board knows that any claim of benefit would require costly outcome trials that they’d rather avoid. Third, the cost comparison table, while readable, conveniently omits the hidden pharmacy markup and insurance co‑pay gymnastics that balloon the $85 figure into something comparable to a small car payment. Fourth, the emphasis on “once‑daily convenience” is a subtle nod to patient adherence studies that demonstrate a mere 10‑15% improvement-hardly worthy of a market‑changing headline. Fifth, the side‑effect profile is downplayed; the flatulence from voglibose is described as a mild inconvenience, but for many, chronic bloating can be socially debilitating. Sixth, the piece neglects the psychosocial impact of injections, framing them as a barrier, while in reality many patients find empowerment in taking control of their therapy via a pen device. Seventh, the mysterious “heart‑failure” exclusion for SGLT2 inhibitors is glossed over, ignoring that those with advanced kidney disease are left with limited options, effectively funneling them toward the combo regardless of its shortcomings. Eighth, the author’s language feels like a script written by corporate marketing, complete with buzzwords like “convenience” and “simplify dosing” that mask the underlying clinical trade‑offs. Ninth, the timing of this article’s release coincides suspiciously with the upcoming patent expiry of one of the combo’s components-clearly a strategic move to boost sales before generics flood the market. Tenth, the article’s “quick takeaways” claim to be comprehensive, yet they omit discussion of lifestyle interventions, dietary counseling, and exercise-key pillars that could reduce reliance on any drug regimen. Eleventh, the table’s monetary values are presented in US dollars without adjusting for international purchasing power, rendering the cost analysis irrelevant for a global audience. Twelfth, the lack of discussion around patient-reported outcomes is a glaring omission, suggesting the authors care more about HbA1c numbers than real‑world quality of life. Thirteenth, the piece mentions “flatulence” as a side‑effect but fails to acknowledge the social stigma and potential impact on mental health. Fourteenth, the article’s tone is overly optimistic about the combo’s “average HbA1c reduction”, ignoring that individual variability can make that average misleading for many patients. Fifteenth, the final recommendation algorithm is simplistic, reducing complex clinical decision‑making to three dropdown menus-an oversimplification that could mislead patients into self‑prescribing without proper medical supervision. In short, this article is a masterclass in marketing masquerading as education, and readers would do well to approach it with a healthy dose of skepticism.
October 16, 2025 AT 05:41
Robert Jackson
Now that Hoyt has painted the combo as theatrical drama, i see the point that flexibility matters more. The lack of CV benefit is a real issue. Patients deserve a clear view of pros and cons.
October 17, 2025 AT 09:27
Maricia Harris
Jonathan’s calm vibe is nice but the reality is messy. Not all pills are so simple.