Every year, the FDA issues dozens of safety notices about medications you or someone you care about might be taking. These aren’t ads. They aren’t rumors. They’re official updates from the U.S. Food and Drug Administration about real risks, new side effects, or changes in how a drug should be used. But if you’ve ever opened one and felt lost, you’re not alone. The language is dense. The format is technical. And the stakes? High.
What Are FDA Safety Communications?
FDA Drug Safety Communications are official updates about medication risks after a drug has been approved and is already on the market. Think of them as the FDA’s way of saying, "We’ve seen something new-and we think you need to know." These aren’t about drugs that failed testing before launch. They’re about things that showed up only after thousands or millions of people used the medicine.
Since 2007, the FDA has had more power to track these issues through programs like the Sentinel Initiative, which uses real-world health data from millions of patients. Each year, they issue between 50 and 70 of these communications. Some are urgent. Others are informational. But all of them matter.
How to Spot the Most Important Parts
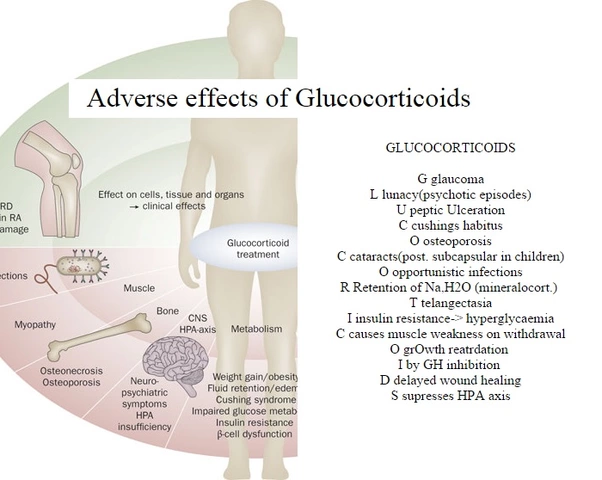
Not every line in an FDA communication is equally important. The key is knowing where to look. Start with the Boxed Warning. This is the FDA’s highest-level alert. It’s called that because it’s printed in a bold, bordered box at the top of the prescribing information. If a drug has a Boxed Warning, it means there’s a serious, potentially life-threatening risk-like liver damage, heart problems, or suicidal thoughts.
Next, check the Warnings and Precautions section. This lists other risks that aren’t as severe but still need attention. Then look at Dosage and Administration. Changes here mean how you take the drug might need to change-like avoiding certain foods, adjusting the dose, or stopping it slowly instead of all at once.
For example, in a July 2025 update on opioid painkillers, the FDA changed the wording from "Do not abruptly discontinue" to "Do not rapidly reduce or abruptly discontinue." That tiny change meant doctors now had to warn patients not to cut doses too fast-even if they felt better-because sudden withdrawal could trigger seizures or severe pain.
Read the ‘For Patients’ Section
Every FDA safety communication includes a section called For Patients. This is written in plain language, not medical jargon. It tells you what you need to do-right now.
Here’s what to look for:
- Do you need to stop the medicine? If it says "STOP using this medication immediately," call your doctor or go to the ER.
- Do you need to talk to your doctor? Phrases like "Discuss the risks and benefits with your provider" mean don’t change anything on your own.
- Do you need to read the Medication Guide? The FDA requires this one-page sheet to come with every prescription. It explains side effects, storage, and what to do in an emergency. Read it every time you refill-even if you’ve taken the drug for years.
A 2022 safety alert for the cancer drug Copiktra told patients: "Read the Medication Guide every time you get a new prescription." Why? Because the risks changed. The guide wasn’t the same as last year.
Understand the Difference Between Alerts and Communications
Not all FDA notices are the same. There are three main types:
- Drug Safety Communications - Full, detailed updates with labeling changes. These are the ones you should read carefully.
- Drug Alerts - Short, urgent notices. These might say something like, "One batch of this drug was contaminated." They’re not about long-term risks, just immediate problems.
- Labeling Changes - These are the actual updated instructions that pharmacies and doctors must follow. They’re often buried in the FDA’s database but referenced in the safety communication.
Patients often confuse Drug Alerts with full Safety Communications. One survey found 63% of patients thought a short alert about a packaging error meant the drug itself was dangerous. It didn’t. Always check the source. If it says "Drug Safety Communication" on the header, it’s a major update.
Use the ‘Before and After’ Format
Since 2020, the FDA has started showing exact changes to drug labels. They use bold text for additions and strikethrough for deletions. This makes it easier to see what changed.
For instance, a 2023 update for a diabetes drug changed the warning from:
May cause low blood sugar in elderly patients
May cause severe low blood sugar in elderly patients, especially those with kidney impairment
That’s not just wording. It’s a new risk factor-kidney problems-that wasn’t mentioned before. If you’re over 65 and take this drug, you need to ask your doctor about your kidney function.
What to Do When You See a Safety Alert
Don’t panic. Don’t stop the drug unless told to. Do this:
- Find the For Patients section. What does it say you should do?
- Check the Boxed Warning. Is it new? Did it change?
- Look for the Medication Guide. Is it the same version you have? If not, ask your pharmacist for the latest one.
- Call your doctor or pharmacist. Say: "I just saw an FDA safety alert about my medication. Can we review it together?"
Most changes don’t require immediate action. But they do require awareness. A 2021 study found that 89% of doctors said these alerts were valuable-when they actually read them. The problem? Only 37% did.

How to Stay Updated Without Overwhelming Yourself
You don’t have to check the FDA website every day. Set up alerts:
- Go to fda.gov/drugs/drug-safety-and-availability
- Scroll to the bottom and sign up for email alerts.
- Choose your drug class-like "Opioids," "Antidepressants," or "Diabetes Medications."
- Only get alerts for what matters to you.
Many pharmacies now offer text or email alerts too. Ask yours if they track FDA updates for your prescriptions.
Why This Matters More Than You Think
Medications are safe when used as intended. But the body doesn’t always react the way lab tests predict. Real people have different health conditions, take other drugs, or age differently. That’s why post-market monitoring exists.
Dr. Jerry Avorn from Harvard says these communications are vital-but hard to understand. The FDA admits it. That’s why they’ve started making plain-language summaries in English and Spanish. They’re testing visual charts and tiered info systems to help patients grasp risks faster.
Right now, only 54% of patients fully understand what these alerts mean. The FDA wants to raise that to 75% by 2027. But you don’t have to wait for them to fix it. You can start now.
Common Mistakes People Make
- Ignoring alerts because "I’ve taken this for years." Risks can emerge years later.
- Stopping medication cold turkey because of a scary headline. Always talk to your provider first.
- Believing all alerts are emergencies. Many are just reminders.
- Not checking the Medication Guide. It’s not fluff-it’s the law.
- Waiting for your doctor to bring it up. Most don’t have time. Be your own advocate.
A pharmacist in Charleston told me last month: "I had a patient come in because her blood pressure spiked. She’d been on the same med for five years. We checked the FDA site-there was a new warning about interactions with grapefruit juice. She’d been eating half a grapefruit every morning. That was the cause."
It wasn’t the drug. It was the juice. And she never knew.







November 25, 2025 AT 02:51
Victoria Stanley
Just read the FDA alert about my blood pressure med and realized I’ve been eating grapefruit every morning for 3 years. No wonder my numbers were all over the place. I called my pharmacist right away and they gave me a new Medication Guide. So glad I found this guide - it’s like a cheat code for not accidentally poisoning myself.
November 26, 2025 AT 03:01
Andy Louis-Charles
Boxed warnings = red flag 🚩. I always skip to that first. If it’s there, I don’t touch the drug until I talk to my doc. Simple. No drama. Just safety.
November 26, 2025 AT 13:29
Bartholemy Tuite
Man I swear the FDA writes like they’re trying to lose readers. I read one of these last week and thought I was reading a legal contract written by a robot who hates humans. But then I found the ‘For Patients’ section and it was like someone finally turned on the lights. Plain English? Revolutionary. I showed it to my mum who’s 72 and she actually understood it. She’s been on that diabetes med since 2018 and never knew about the kidney thing. Now she’s getting her levels checked. Small win for humanity.
November 27, 2025 AT 03:04
Alex Dubrovin
Set up the FDA email alerts for my antidepressant last month and got one yesterday about a new interaction with St. John’s Wort. I was taking it for ‘natural anxiety relief’ lol. Stopped it immediately. Thanks for the heads up. This stuff saves lives.
November 28, 2025 AT 00:20
Jacob McConaghy
So many people panic when they see an alert and quit their meds cold turkey. That’s way more dangerous than the alert itself. I’m a nurse and I’ve seen people end up in the ER because they read a headline and thought the whole drug was evil. The real answer? Call your provider. Don’t guess. Don’t Google. Just call. It takes 2 minutes and could save your life.
November 29, 2025 AT 03:09
Natashia Luu
It is profoundly concerning that the general populace continues to treat pharmaceutical safety communications as optional reading material. One cannot, under any reasonable interpretation of medical ethics, afford to neglect such vital regulatory disclosures. The FDA's diligence in disseminating this information is commendable, yet the public's apathy borders on negligent. One must ask: if one cannot be bothered to read a single page, how can one justify continued pharmaceutical consumption?
November 30, 2025 AT 05:43
akhilesh jha
I came across this post because my uncle had a seizure after stopping his seizure med too fast. The FDA alert said ‘do not rapidly reduce’ - he thought ‘don’t stop suddenly’ meant he could cut it in half over a week. He didn’t know ‘rapidly’ meant ‘any change without supervision’. Now he’s on a new plan. I wish someone had explained this to him before. This is life or death stuff and nobody teaches it. Schools should have a class on this. Not just for meds - for all health info.
December 2, 2025 AT 00:54
Jeff Hicken
Why does the FDA even bother with these? Half the people who read this won’t even open the Medication Guide. I got my blood pressure med last week and the guide was 12 pages long. I threw it in the drawer. I mean come on. They’re just trying to cover their asses. If your drug kills someone after 5 years, just pull it already. Stop making us read novels.