Opioid Metabolism: How Your Body Processes Pain Meds and Why It Matters
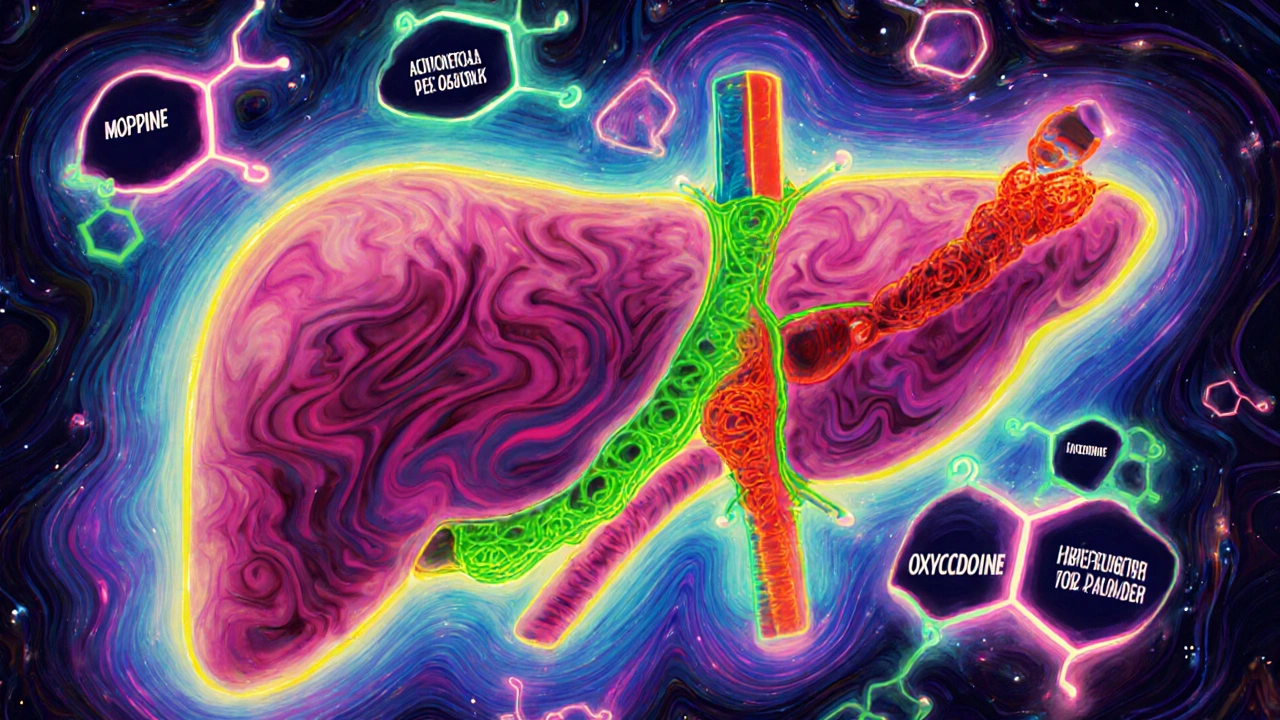
When you take an opioid like oxycodone or hydrocodone, your body doesn’t just absorb it and call it a day. It opioid metabolism, the process by which the liver breaks down opioid drugs into smaller compounds that can be eliminated. Also known as drug metabolism, it’s what decides whether a pill works for you, makes you sick, or does nothing at all. This isn’t just chemistry—it’s personal. Two people taking the same dose of codeine can have wildly different results because of how fast or slow their liver enzymes process it.
The real player here is a group of liver enzymes called CYP3A4, a major enzyme family responsible for breaking down more than half of all prescription drugs, including most opioids. Some people have genes that make CYP3A4 work super fast—those folks might need higher doses to feel pain relief. Others have slow versions, and even a normal dose can build up to dangerous levels. That’s why overdoses happen even when people follow the script. And it’s not just CYP3A4. Other enzymes like CYP2D6 turn codeine into morphine, so if your body does this too well, you could end up with morphine levels that feel like a heroin hit—even if you only took a cough syrup.
That’s where opioid interactions, when other meds or supplements interfere with how opioids are broken down come in. Things like grapefruit juice, certain antibiotics, or even common antidepressants can slow down or speed up metabolism. A simple combo like clarithromycin and oxycodone? That’s a recipe for breathing trouble. Your doctor might not always catch it, because drug labels rarely spell out how metabolism affects you. But if you’ve ever felt dizzy after a new pill, or noticed your pain meds stopped working after starting something else, that’s likely metabolism at work.
It’s not just about safety—it’s about effectiveness. If your body clears opioids too fast, you’ll need more frequent doses. Too slow? You risk sedation, constipation, or worse. That’s why genetic testing for metabolic enzymes is slowly becoming part of pain management. It’s not magic, but it’s smarter than trial and error. And if you’re on long-term opioids, knowing how your body handles them could prevent hospital visits.
Below, you’ll find real-world guides on how medications interact, how to spot dangerous combos, and how to protect yourself from hidden risks. These aren’t theoretical articles—they’re based on actual cases, FDA alerts, and clinical data. Whether you’re managing chronic pain, caring for someone on opioids, or just trying to avoid a bad reaction, what follows will help you ask the right questions and stay in control.
Opioids and Liver Disease: How Impaired Liver Function Changes Pain Medication Risks
Opioids can become dangerously toxic in liver disease due to impaired metabolism. Learn how liver damage alters drug processing, which opioids are riskiest, and how to adjust doses safely to avoid overdose and worsening liver damage.