Obstructive Sleep Apnea: Causes, Risks, and How Medications Affect It
When you have obstructive sleep apnea, a condition where throat muscles relax too much during sleep, blocking airflow and causing repeated breathing pauses. Also known as OSA, it’s not just loud snoring—it’s a silent threat that strains your heart, messes with your metabolism, and can make other medications dangerous. If you’re on painkillers, antidepressants, or even allergy meds, those drugs might be making your sleep apnea worse without you realizing it.
People with liver disease, a condition where the liver can’t properly break down drugs are especially at risk. Medications like opioids or sedatives hang around longer in the body when the liver is damaged, increasing the chance of airway collapse at night. That’s why opioid metabolism, how the body processes pain drugs like morphine or oxycodone matters so much—if your liver is slow, those drugs can turn your sleep apnea into a life-threatening situation. Even common antibiotics like clarithromycin can interfere with blood pressure meds, causing dizziness or low blood pressure that disrupts sleep patterns and makes OSA harder to manage.
Weight loss is the most effective way to improve obstructive sleep apnea, but it’s not always easy. Many people with OSA also struggle with fatty liver disease, a condition where fat builds up in the liver, often tied to obesity and insulin resistance. The same lifestyle changes that help your liver—eating less sugar, moving more, losing weight—also reduce throat fat and open your airway. New drugs like semaglutide, originally for diabetes and weight loss, are now being used to treat both conditions at once. But even these can interact with other meds, so knowing what you’re taking and why matters.
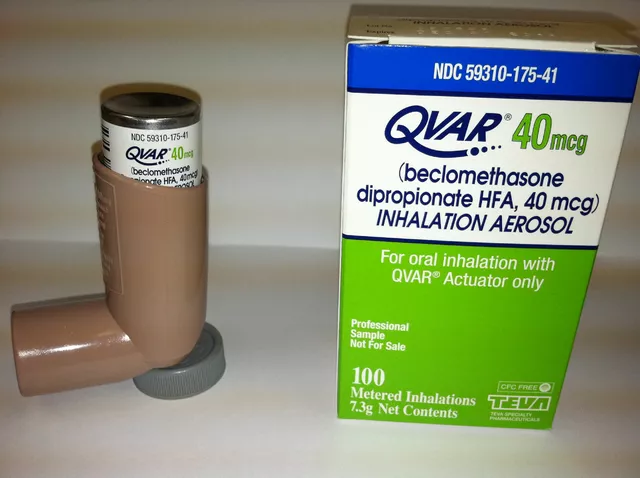
It’s not just about pills. Sleep apnea can be made worse by antihistamines, muscle relaxants, and even some herbal supplements. St. John’s Wort, ginkgo, or melatonin might seem harmless, but they can interfere with your breathing control or deepen sleep too much. And if you’re using nasal sprays or allergy meds like Claritin or Zyrtec, those might help you breathe better during the day—but not at night if your airway is physically blocked.
You don’t have to live with gasping for air every night. The right diagnosis, the right habits, and the right meds can change everything. Below, you’ll find real, practical advice from people who’ve been there—how to spot dangerous drug interactions, what treatments actually work, and how to protect your health when sleep is under attack.
Supine vs. Side Sleeping: Which Position Is Better for Sleep Apnea?
Side sleeping can dramatically reduce sleep apnea events for those with positional OSA. Learn how positional therapy works, how it compares to CPAP, and which methods actually help people stick with treatment long-term.
Weight Loss and Sleep Apnea: How BMI Directly Impacts CPAP Pressure Needs
BMI directly affects how much pressure your CPAP machine needs to treat sleep apnea. Losing even 10% of your body weight can significantly reduce your AHI and lower CPAP pressure-sometimes eliminating the need for it entirely.