If you’ve ever had sudden, intense pain under your right ribs that came out of nowhere and lasted for hours, you might have experienced biliary colic. It’s not gas. It’s not indigestion. It’s your gallbladder screaming because a stone got stuck. And if that stone doesn’t move, things can get serious-fast.
About 10 to 15% of adults in the U.S. have gallstones. But here’s the twist: 80% of them never feel a thing. They live their whole lives without knowing they’re carrying them. The problem starts when those stones block the ducts that carry bile out of the gallbladder. That’s when pain hits, and complications like cholecystitis or pancreatitis can follow.
What Happens When a Gallstone Gets Stuck?
Biliary colic isn’t a disease-it’s a symptom. It happens when a gallstone temporarily blocks the cystic duct, the pipe that lets bile flow out of the gallbladder. When that happens, the gallbladder contracts hard trying to push bile through, but nothing moves. The result? Sharp, steady pain in the upper right abdomen or just below the breastbone. It usually starts suddenly, peaks within an hour, and lasts 1 to 5 hours. It doesn’t get better with burping, vomiting, or going to the bathroom. And it doesn’t come and go like a stomach virus.
Most stones are made of cholesterol (80% of cases in Western countries). The rest are pigment stones, made from bilirubin. These form when bile doesn’t empty properly, or when your liver dumps too much cholesterol or bilirubin into bile. Obesity, rapid weight loss, pregnancy, and being over 40 all raise your risk. Women are 2 to 3 times more likely to get them than men.
When Biliary Colic Turns Into Cholecystitis
If the stone doesn’t move after several hours, the gallbladder gets inflamed. That’s acute cholecystitis. It’s no longer just pain-it’s infection. Fever, nausea, vomiting, and tenderness when you press on your right side are signs. The gallbladder swells, and bacteria from the gut can creep in. Left untreated, it can rupture. That’s an emergency.
Studies show about 20% of people who have one episode of biliary colic will develop cholecystitis. And if you’ve had one episode, there’s a 90% chance you’ll have another within 10 years. Two out of three will have a second episode within just two years. That’s not luck. That’s a ticking clock.
Complications don’t stop there. Stones can slip into the common bile duct, blocking it and causing jaundice (yellow skin), dark urine, and pale stools. Or they can block the pancreatic duct, triggering pancreatitis-a dangerous inflammation that can be life-threatening. The NHS reports that 20 to 30% of people with untreated symptomatic gallstones end up in the hospital within five years.
How Doctors Diagnose It
It starts with symptoms. But confirmation? That’s usually an ultrasound. It’s quick, safe, and picks up stones in over 95% of cases. If there’s doubt, doctors might order a CT scan or an MRCP (magnetic resonance cholangiopancreatography) to see the bile ducts in detail. Blood tests can show signs of infection or liver stress-elevated liver enzymes, white blood cell count, or bilirubin levels.
But here’s the problem many patients face: diagnostic delays. A 2022 Healthline survey found 41% of people saw three or more doctors before getting the right diagnosis. Pain gets written off as acid reflux. Or blamed on stress. Or dismissed as "just aging." By the time the right test is ordered, the gallbladder is already inflamed.
Can You Dissolve Gallstones Without Surgery?
Yes-but only sometimes.
The drug ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones over 6 to 24 months. But it works in only 30 to 50% of cases. And even if it does, half of those stones come back within five years. It’s not a cure. It’s a temporary fix, usually only offered to people who can’t have surgery.
Shock-wave lithotripsy-breaking stones apart with sound waves-used to be popular in the 1990s. But it required multiple sessions, expensive equipment, and still left fragments that could re-form stones. Today, it’s rarely used. The recurrence rate is too high.
There’s also no proven benefit from herbal remedies, apple cider vinegar, or gallbladder flushes. These aren’t just ineffective-they can be dangerous. Pushing stones around without medical supervision can cause blockages, infection, or even pancreatitis.
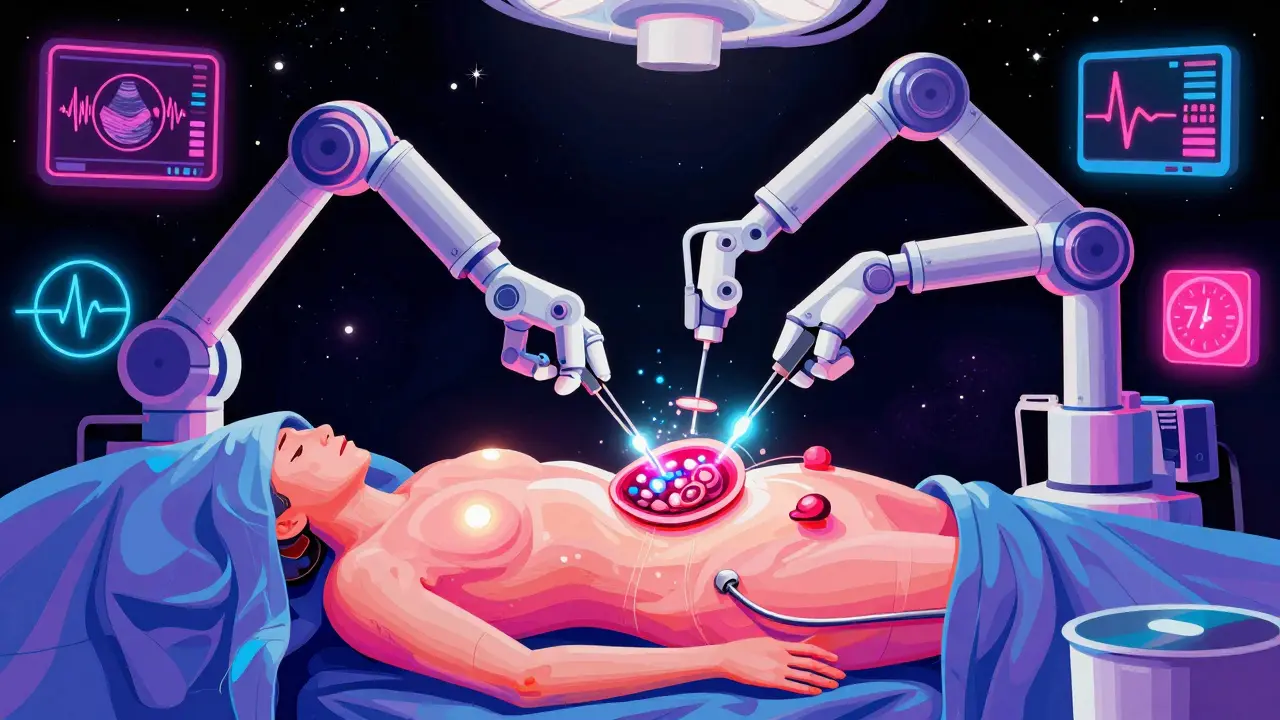
The Gold Standard: Laparoscopic Cholecystectomy
For most people with recurrent biliary colic or cholecystitis, surgery is the only real solution. And the standard procedure? Laparoscopic cholecystectomy.
This isn’t open surgery with a big cut. It’s four small incisions. A camera and tools go in. The gallbladder is carefully detached and removed. In the U.S., 90% of gallbladder removals are done this way. Why? Because it works.
- Average hospital stay: 1.2 days (vs. 4.7 days for open surgery)
- Recovery time: 7 days (vs. 30 days)
- Return to work: Often within a week
- Complication rate: Below 2% in experienced hands
According to Dr. David Flum of the University of Washington, laparoscopic cholecystectomy has a 95% patient satisfaction rate. People don’t just stop having pain. They stop worrying about it. They eat normally again. They sleep through the night.
But timing matters. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) says if you have acute cholecystitis, surgery should happen within 72 hours. Delaying increases the chance the surgeon will have to switch to open surgery-from 25% down to just 7% when done early.
Who Shouldn’t Have Surgery?
Surgery isn’t for everyone. For healthy people under 75, the risks are very low. But for older adults with multiple health problems-heart disease, diabetes, lung disease-the risk changes.
Dr. Emily Finlayson from UCSF points out that 30-day mortality for cholecystectomy jumps from 0.1% in healthy patients to 2.8% in those with three or more serious conditions. That’s why doctors now assess each person individually. A 78-year-old with diabetes and COPD might be better off with temporary drainage (like a tube placed through the skin into the gallbladder) and later surgery, if they recover enough.
There’s also a new option: endoscopic ultrasound-guided gallbladder drainage. The FDA approved it in 2023. It’s not a cure, but it’s a bridge. It relieves infection without cutting out the gallbladder-useful for people too sick to handle surgery right away.
What Happens After Surgery?
Most people go home the same day or the next morning. You’ll be up and walking within 4 hours. You’ll start sipping water within 6 hours. No IVs. No catheters. No long bed rest.
Some people have loose stools after surgery. About 12% report diarrhea, especially after fatty meals. That’s because bile flows directly into the intestine now, instead of being stored. It usually improves over weeks or months. A few (6%) develop post-cholecystectomy syndrome-ongoing pain, bloating, or nausea. Often, it’s not from the surgery, but from another issue like SIBO or IBS that was masked by the gallstones.
One patient from Cleveland Clinic had 17 episodes of biliary colic over 18 months. After surgery, her pain vanished in 10 days. She was back to hiking and working full-time in two weeks.
The Bigger Picture: Why This Matters
More than 700,000 gallbladder surgeries are done in the U.S. every year. That’s $6.2 billion in costs. And the numbers are rising. Obesity rates are up. People are living longer. And with age comes more gallstones.
Women, especially those who’ve had children, are at highest risk. Hispanic populations have a 45% higher incidence than non-Hispanic whites. That’s not random-it’s tied to diet, genetics, and access to care.
There’s a new trend: single-incision laparoscopic surgery (SILS). It leaves one tiny scar. But it’s harder to do, takes longer, and has a 20% higher complication rate than standard laparoscopy. For now, it’s not the standard.
What’s changing? Recovery protocols. Hospitals are using ERAS (Enhanced Recovery After Surgery) pathways. They get you up faster, feed you sooner, and reduce pain with non-opioid meds. In hospitals using ERAS, hospital stays dropped 30%, and readmissions dropped 25%.
One thing won’t change: surgery remains the best option. Despite advances in pills and drainage, nothing matches the long-term safety and effectiveness of removing the gallbladder when it’s causing problems.
What Should You Do?
- If you’ve had one episode of biliary colic, don’t wait. Talk to a surgeon. The odds of recurrence are high.
- If you have cholecystitis, get surgery within 72 hours. Delaying makes it harder and riskier.
- If you’re over 75 with other health problems, ask about alternatives-but don’t assume surgery is off the table. Many older patients do very well.
- Don’t try home remedies. They don’t work. And they can hurt you.
- If you’re scared of surgery, ask about the procedure. Laparoscopic cholecystectomy is routine. Most people say they wish they’d done it sooner.
Gallstones aren’t a death sentence. But they’re not something you should ignore. The pain is real. The risk is real. And the solution? It’s simple, safe, and life-changing.