Imagine being told your bones are thinner than they should be. Suddenly, a slip on the steps or tripping over your dog's leash might mean more than bruises—it could mean a broken hip or wrist. That's not just a scary thought for your grandparents. Osteoporosis affects men and women, young and old, and it’s sneaky because you don’t usually feel it until something goes wrong. Here’s where Fosamax steps in, not as a magic fix, but a real lifeline for folks trying to keep their bones solid and avoid hospital visits nobody wants. The real kicker? Most people have no idea how this pill works or what to watch out for. I’ve had neighbors, parents at my kids’ school, even the gym crew, ask about it. So let’s untangle the facts and help you figure out if this little white tablet belongs in your day-to-day routine.
What Is Fosamax, and Who Really Needs It?
Fosamax, known by its science name alendronate, is all about bones. If your doctor mentions bone density, osteopenia, or osteoporosis, this medication probably pops up. It’s not something you grab off the shelf; you need a prescription, usually after a bone density scan (like a DEXA scan) shows your skeleton’s taking a hit. You’ll mainly hear about it for treating postmenopausal women, but plenty of men—and even some younger adults on long-term steroids or with certain medical conditions—land on it, too.
So what’s happening inside you? After a certain age (sometimes sooner, if you’re drawn the short straw genetically), your body starts stealing calcium from your bones faster than you can rebuild it. Think termites versus construction crew. Fosamax slows down those bone-eating termites. It belongs to the bisphosphonate family—meds famous for putting the brakes on the cells that break down bone, called osteoclasts. Studies back up its success: People on Fosamax can slow down and sometimes even reverse bone loss, slashing their risk of spine and hip fractures by 48% in just a year or two, based on big-number trials from the past two decades.
If your history includes smoking, not eating enough calcium, family members snapping their bones, taking certain meds (like steroids), or even just being on the lighter, smaller side (yep, being petite is a risk), you’re in the possible-Fosamax club. But here’s an interesting twist: Not everyone with “bad” bone scans gets put on it. Doctors weigh your fracture risk, your age, and your health history before writing that script. It’s not for those with certain esophagus issues or folks who can’t sit up for half an hour after swallowing a pill.
Beyond osteoporosis, doctors sometimes use Fosamax for rare bone diseases like Paget’s disease or to counteract bone weakening during certain cancer treatments, but those aren’t the big reasons most people hear about it. Basically, if the word “fragility fracture” scares you anywhere near as much as it did my Aunt Susan, it’s worth learning if you fit the profile.
How Does Fosamax Work Inside Your Body?
So, you pop the pill and think it just makes your bones harder, right? Not exactly. It does the heavy lifting by blocking the faulty bone-breakdown crew (osteoclasts) so your body can start patching up the old framework without tearing stuff down as fast. Visualize a construction job where demolition stops but repair keeps going—that’s Fosamax in action.
The twist? You need to take this pill on an empty stomach with plain water, then stay upright for at least 30 minutes. This isn’t just medical bossiness—it’s because Fosamax can irritate your food pipe (esophagus) if it doesn’t slide straight into your stomach. No coffee, juice, or breakfast until the half-hour clock runs out, or it might not absorb properly.
The science here actually gets kind of cool. Your bones are made up of living tissue, not just dead calcium rocks, and they’re constantly being torn down and rebuilt—a process called remodeling. In osteoporosis, that balance gets thrown off. Fosamax is designed to lock itself onto bone surfaces, where it sits like a guard. When the overactive bone-removal cells show up, they basically swallow the drug and—poof—slow down or die. That lets your body’s bone-building cells catch up and beef up your skeleton again. After a few months, bone density numbers noticeably tick up if you’re sticking with the plan.
One overlooked detail: Fosamax sticks around in your bones for years. Even a “drug holiday” later (doctors love to suggest these to avoid rare long-term risks), the effects keep working. Don’t expect to “feel” anything right away—no one wakes up with thicker bones overnight. But with regular scans, the numbers often improve, making it one of the more satisfying medications for both doctors and patients in terms of measurable results.
The trickiest part is the daily or weekly ritual. Forgetting instructions can mean less benefit or more stomach trouble. Some folks keep the bottle next to the coffee maker as a morning reminder, but just watch those first sips! Success with Fosamax is annoyingly dependent on sticking to the rules, but thankfully, a few weeks of habit-building usually does the trick.

Possible Side Effects: The Facts You Really Need to Know
No pill is perfect, and Fosamax has its list of weird and not-so-weird side effects. Top of the list: it can cause irritation in your esophagus (the tube from mouth to stomach), which is why staying upright and using just water is non-negotiable. Some people feel queasy, burp a lot, or notice heartburn, especially early on.
Muscle aches, joint pain, and plain old discomfort are next up, usually in the legs or back. I’ve heard people say it feels like “bad flu body aches,” but thankfully those often fade. One rare, scary side effect is something called osteonecrosis of the jaw—basically jawbone dying off, often tied to dental work. Sounds horrifying, but the odds are about as likely as hitting it big in the slots (especially if you take care of your teeth and tell your dentist you’re on Fosamax).
Breaking your thigh bone in an odd way (femur fractures) also makes headlines, but this isn’t common either, especially if you’re only on Fosamax for five years or less. Your doctor will probably suggest a “holiday” (break from the drug) after a few years to lower this risk.
Stomach upset, acid reflux, and bone/joint pain are what make some people quit early, but tricks like always taking it first thing in the morning, then eating something after your 30-minute wait, help a lot. Still, if you ever feel chest pain, difficulty swallowing, or severe bone pain, that’s a hard stop—call your doc, pronto.
Most side effects are uncomfortable more than dangerous. There’s actually a study from Massachusetts General demonstrating that only about 1-2% of patients ever develop serious problems with long-term use, and the bone-saving benefits usually far outweigh those risks. Instead of worrying, talk openly with your doctor about what matters to you: Are you toughing it out to avoid a hip fracture, or already struggling with stomach issues before you started? Tailoring your approach makes a huge difference. Mindset matters, too. If you expect misery, every twinge feels worse. But going in prepared helps most people do fine.
Practical Tips for Getting the Most from Fosamax
Don’t just swallow the pill and hope for the best. There’s an art to doing this right and protecting your bones. First, never skip the fasting part—no food, coffee, or meds before taking Fosamax, and definitely stick with a big glass of plain water.
That upright rule isn’t just for show. Lying down or even lounging in a recliner too soon can land you with a raging case of heartburn or worse. Many friends have told me setting a phone timer helps—30 minutes, then they can eat. If you forget, just restart the process the next day. Missing a single dose isn’t the end of the world, but don’t double up the next morning.
If you take a weekly version of Fosamax (like many people do for convenience), pick a memorable day—“Fosamax Fridays” has a nice ring, right? Mark it on your calendar, and make that day’s breakfast something you look forward to so you won’t skip by accident.
Don’t forget about your mouth. Dentists in Charleston (and probably everywhere else) tend to look a little worried when they hear “bisphosphonate,” so keep your teeth and gums healthy, and tell your dental provider you’re on Fosamax before any procedures. If you need something like a tooth pulled, discuss the timing with your medical team first—sometimes pausing the med is safest.
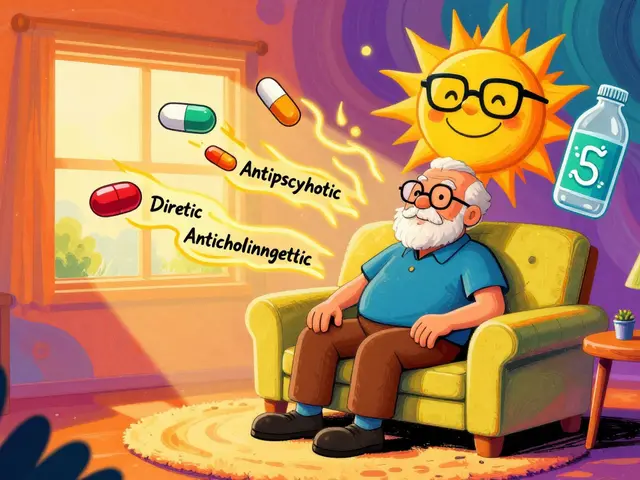
Keep your bones happy by feeding them calcium and vitamin D, too. Fosamax works better if your system’s got the building blocks to rebuild bone. That means dairy, leafy greens, or supplements if you can’t get enough in your diet. The official target is about 1200 mg calcium and 800-1000 IU of vitamin D per day, depending on your age and sex. Sunlight always helps (if you can wrangle it between spring storms or summer heat waves in South Carolina).
Exercise doesn’t just keep you in shape for chasing the dog around or wrangling kids on the beach—it literally stimulates stronger bone growth. Weight-bearing moves like walking, dancing, or even gardening with some solid digging count. Sitting on the couch won’t do much for your skeleton, so build physical activity into your routine alongside the pill.
And check in with your doctor at least once a year (usually more often at first). They’ll want to order labs, maybe more bone scans, and talk about whether you’re ready for a drug holiday.

Real Stories, New Research, and What’s Ahead for Osteoporosis Treatment
When my neighbor, Jane, first got her prescription for Fosamax, she was more worried about her morning coffee ritual than her actual bones. After a few weeks, her aches faded, and her next scan looked way better. She swears by her morning stretching routine as a distraction while she waits out the pill timer. But not everyone glides through it. My own uncle quit after three months—he hated the stomach issues and only really got motivated again after he watched another friend go through a bad hip fracture and the long, painful rehab. It seems downright unfair that bone strength isn’t something you can see in the mirror or feel right away, but the stories behind every prescription are more common than you’d guess.
Dig around the medical journals and you’ll see a ton of buzz about newer osteoporosis drugs, “anabolic” treatments that actually build bone instead of just slowing loss, and better ways to predict who gets fractures. But while new options—like denosumab (Prolia), teriparatide (Forteo), and even one-and-done treatments—are getting more common, they don’t suit, or work for, everyone. Fosamax still has the long-term track record, especially for first-timers and people at high fracture risk. And it’s much more affordable, especially for folks dealing with insurance headaches.
Recent research out of Stanford highlighted something surprising: after two to five years of consistent Fosamax use, most people can stop for a while (“drug holiday”) and not lose a ton of bone. That’s good news if you’re nervous about those rare side effects but want to keep your skeleton sturdy. But doctors do warn—the older and frailer you are, the more careful they have to be about these breaks.
Where’s it all heading? Experts predict even more tailored risk calculators, smarter scans, and safer drug combos ahead. But for now, getting a handle on your real fracture risk is step one. If you’re using Fosamax, stay engaged with your health, speak up about side effects, and don’t be shy about asking if it’s time for another scan. Ask that doctor for the numbers—what’s your actual fracture risk next year, compared to national averages? Numbers feel more real than just “safe” or “risky.”
If you’re caring for someone—a parent, a partner, or just watching out for those bony pets running around (well, maybe not your husky, Baloo, or canary, Tweety)—help them stick with routines, and be the reminder they need on those early mornings. Safe bones mean more summers chasing kids, hiking, or climbing up to fix the Christmas lights. That’s worth every awkward breakfast, if you ask me.







May 30, 2025 AT 07:00
California Daughter
I don't get why everyone treats Fosamax like it's the holy grail. My mom took it for two years and ended up with a fractured hip anyway. Turns out, all that 'bone density improvement' was just numbers on a screen. Real life? She still can't climb stairs without a cane. And don't even get me started on the jaw thing-my dentist almost had a heart attack when she found out she was on it. Just saying, maybe we're overmedicating people who just need more vitamin D and less soda.
May 30, 2025 AT 15:46
Shanna Talley
You know what's beautiful about this post? It doesn't scare you-it empowers you. Bone health isn't about fear, it's about showing up for yourself every day. Whether it's the 30-minute wait after your pill or choosing a walk over scrolling, these tiny acts add up. You're not just taking a pill-you're choosing to keep dancing with your grandkids. That’s worth every awkward morning. Keep going. You've got this.
May 31, 2025 AT 02:25
Samuel Wood
Fosamax is just a bandaid for a lifestyle failure. If you're not eating real food, moving your body, or getting sun, you're just buying a placebo with side effects. And the fact that people think this is normal? Pathetic. I mean, really? We've reduced human health to a pill schedule? I'm not even mad, just disappointed. Also, 'alendronate' is spelled wrong in the post. Lol.
May 31, 2025 AT 08:42
ridar aeen
I don't care what the studies say. I've seen too many people get ruined by these drugs. The jaw necrosis stories? Real. The femur fractures? Not rare. And now they want us to just 'take a holiday'? Like we're on a vacation from our own skeletons? No thanks. I'd rather be weak and alive than strong and broken. This isn't medicine, it's a gamble with your body.
June 2, 2025 AT 00:25
chantall meyer
In South Africa, we don't have access to this. We have sunlight, milk, and tradition. Your pharmaceutical industry is selling fear to sell pills. Bone density scans are overrated. My grandmother lived to 98, never took a pill, and never broke a bone. She danced every Sunday. Maybe your problem isn't your bones-it's your lifestyle. Or your doctor's commission.
June 3, 2025 AT 08:01
Lorne Wellington
Hey everyone, just wanted to say-this post is gold 🌟 Seriously. I'm a physio in Vancouver and I see people every week who are terrified of falling. Fosamax isn't perfect, but it’s one tool in the toolbox. Pair it with weights, vitamin D, and a good pair of shoes (no flip-flops on icy sidewalks, please 😅). And yes, the 30-minute rule? Non-negotiable. I’ve had patients show up with heartburn because they took it with tea. Don’t be that person. You got this.
June 4, 2025 AT 05:49
Will RD
Fosamax is a scam. People take it because they're scared. The real problem? Doctors push it too hard. I know a guy who took it for 10 years and then broke his femur. Coincidence? I think not. Stop listening to pharma ads. Eat more protein. Lift things. Walk. That's it. No pills needed.
June 4, 2025 AT 19:03
Jacqueline Anwar
I find it deeply concerning that this article casually mentions 'drug holidays' as if they're a benign afterthought. Osteonecrosis of the jaw is not a side effect-it is a catastrophic, disfiguring, and often irreversible condition. And yet, here we are, normalizing it with phrases like 'rare as hitting the lottery.' This is not a lottery. This is your jaw. Your mouth. Your ability to eat. Your dignity. Please, for the love of all that is medical ethics, stop minimizing this.
June 4, 2025 AT 22:43
Ganesh Kamble
Lol why are we even talking about this? It's just a pill. The real issue is that people are too lazy to move. I've seen 70-year-olds on Fosamax still sitting on the couch watching Netflix. You can't out-drug a sedentary life. Also, the whole 'stay upright for 30 minutes' thing? That's just a way for Big Pharma to make you feel guilty. Do you really think they care if you get heartburn? Nah. They want you to keep buying.
June 6, 2025 AT 20:59
Jenni Waugh
Let me just say-this isn't about bones. This is about autonomy. Who gave doctors the right to decide when your body is 'too weak'? Who decided that a number on a scan is more important than how you feel? I've seen women take Fosamax and become paralyzed by fear. They stop gardening. Stop hiking. Stop living. The pill doesn't fix fear. It just makes you pay for it. And now we're talking about 'drug holidays' like we're on a corporate retreat? Wake up. Your body isn't a spreadsheet.
June 7, 2025 AT 18:35
Theresa Ordonda
I took Fosamax for 3 years. 😔 The jaw thing? Didn't happen. The stomach? Yeah, but I learned to take it with a full glass of water and just… wait. My bone density went up 8%. I didn't break anything. My mom did. So yeah, it worked for me. But I also do yoga, eat kale, and yell at my cat to stop jumping on the bed. It’s not just the pill. It’s the whole damn package. 🙃
June 9, 2025 AT 15:08
Judy Schumacher
This entire post is a masterclass in pharmaceutical propaganda. You mention 'studies' but don't cite them. You cite '48% reduction in fractures' without clarifying if that's relative or absolute risk. You normalize the idea that a pill can replace movement, sunlight, and nutrition. You're not educating-you're selling. And the fact that people are swallowing this (literally and figuratively) without question? That's the real osteoporosis. A crisis of critical thinking.
June 11, 2025 AT 07:36
Megan Raines
I read this whole thing. Then I went to the bathroom and looked in the mirror. My bones are still there. Still kinda weak. Still not broken. Still not on Fosamax. I think I'm okay. Maybe I just need more sunlight and less anxiety. Or maybe I'm just lucky. Either way, I'm not rushing to the pharmacy.
June 12, 2025 AT 13:27
Mamadou Seck
Fosamax works fine if you dont have a stomach. But if you do? Good luck. I took it for a month and felt like I swallowed glass. My doctor said 'its normal' so I kept going. Then I broke my wrist falling off a chair. Not from osteoporosis. From being dizzy from the pill. So yeah. I stopped. Now I eat yogurt and walk. And I dont feel like I'm being slowly poisoned. Thats my story.