If you have an autoimmune disease, you know that fatigue isn’t just being tired after a long day. It’s the kind of exhaustion that makes getting out of bed feel like climbing a mountain. It doesn’t go away with sleep. It doesn’t improve with coffee. And no one else can see it - which is why so many patients feel dismissed, ignored, or even blamed for being lazy. But this fatigue isn’t psychological. It’s biological. And it’s one of the most common, most disabling symptoms of autoimmune conditions - affecting 98% of people with diseases like lupus, rheumatoid arthritis, multiple sclerosis, and Sjögren’s syndrome.
Why Your Fatigue Isn’t Normal
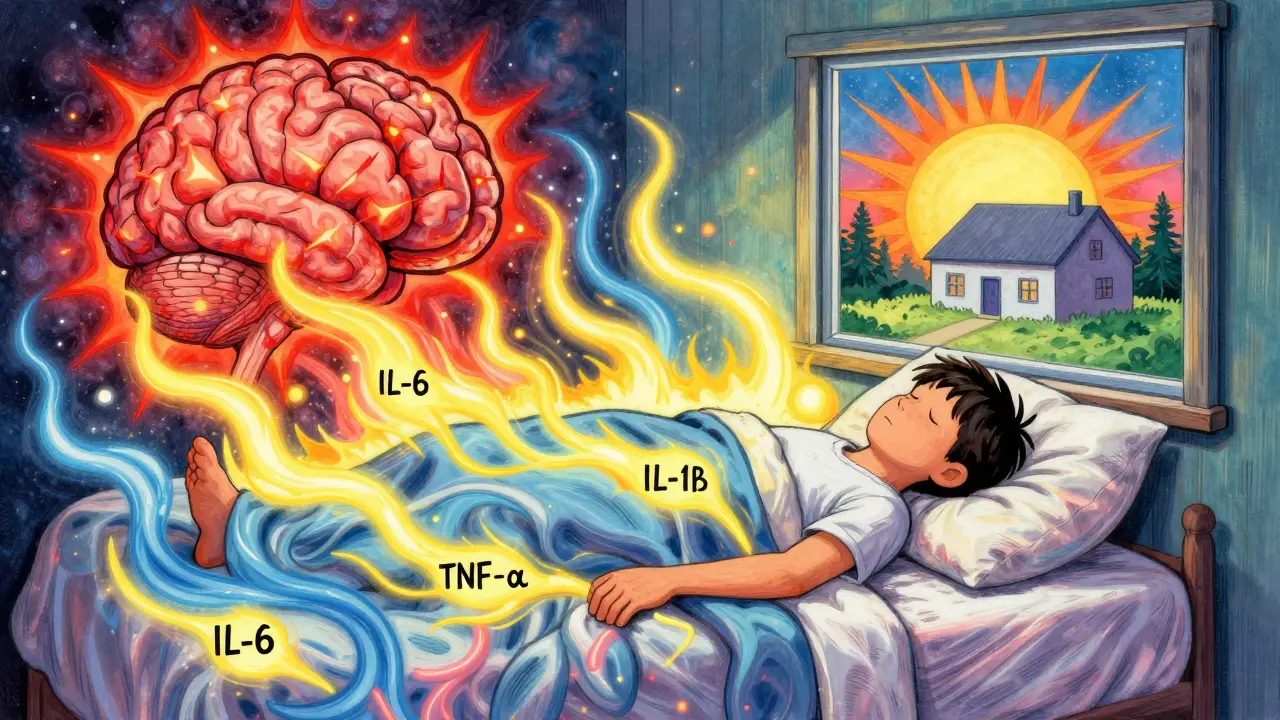
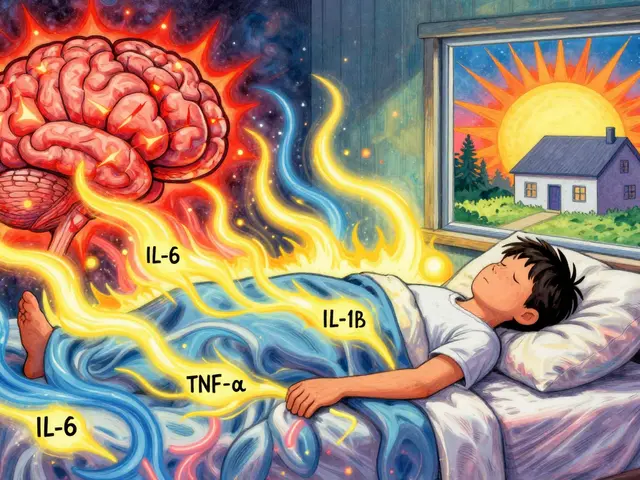
Ordinary tiredness comes from lack of sleep, stress, or physical exertion. It fades after rest. Autoimmune fatigue doesn’t. It’s deep, constant, and often hits you even when you haven’t done anything. You might wake up after eight hours of sleep and still feel like you’ve run a marathon. Simple tasks - making coffee, answering emails, walking to the mailbox - leave you drained for hours. Research shows this isn’t just in your head. Blood tests reveal that people with autoimmune fatigue have 2.3 to 3.7 times higher levels of inflammatory proteins like IL-1β, IL-6, and TNF-α than healthy people. These aren’t just markers - they’re active players. They cross the blood-brain barrier and trigger neuroinflammation, directly messing with the brain’s energy circuits. MRI scans show visible inflammation in the brains of 82% of patients with severe autoimmune fatigue. Your brain isn’t lazy. It’s under siege. There’s also a problem with your body’s stress response. The HPA axis - the system that controls cortisol, your natural energy hormone - is often blunted in autoimmune patients. Studies show a 18-22% drop in cortisol awakening response. That means your body doesn’t ramp up energy properly in the morning. Add to that disrupted melatonin rhythms (37% lower amplitude), and you’ve got a circadian system that’s out of sync. No wonder you feel wired at night and wrecked during the day. And then there’s your mitochondria - the power plants in your cells. In 65% of autoimmune fatigue cases, they’re not producing energy efficiently. Muscle biopsies show 40-55% less ATP production. That’s like having a car with a half-dead battery. Even small movements drain you because your cells can’t generate enough fuel.It’s Not Just About Disease Activity
You’d think that if your lupus or RA is under control, your fatigue would improve. But that’s not how it works. Studies show only a moderate correlation (r=0.38) between traditional disease activity scores and fatigue levels. You can have low inflammation on blood tests and still feel completely wiped out. Or you can have high disease activity and feel surprisingly okay. This disconnect is why many doctors miss the mark. They treat the disease - not the fatigue. But fatigue has its own pathway. In lupus, fatigue correlates more strongly with anti-dsDNA antibody levels than with joint swelling. In MS, it’s linked to lesions in the thalamus, not the number of relapses. In rheumatoid arthritis, fatigue often ranks as the most disabling symptom - even above pain. That’s why tools like the Multidimensional Fatigue Inventory (MFI-20) and the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) exist. A score above 18.7 on the MFI-20 or below 34.5 on the FACIT-F means your fatigue is clinically significant. Yet, only 12% of rheumatologists routinely use these tools. Most still ask, “How tired are you on a scale of 1 to 10?” - and move on.How Different Autoimmune Diseases Affect Fatigue
Not all autoimmune fatigue is the same. The severity and pattern vary by condition:- Systemic Lupus Erythematosus (SLE): 98% of patients report fatigue. Many describe it as “bone-deep,” with 70% saying it interferes with work or daily life.
- Multiple Sclerosis (MS): 96% experience fatigue. It often hits midday, unrelated to activity. Post-exertional malaise is common - a crash 12-48 hours after even light effort.
- Rheumatoid Arthritis (RA): 94% report fatigue. For 63% of RA patients, it’s worse than joint pain. Fatigue correlates with DAS-28 scores, but not perfectly.
- Sjögren’s Syndrome: 92% have fatigue, and it’s often the most severe. One study found 78% rated their fatigue as 8 or higher on a 10-point scale.
- Celiac Disease: 90% report fatigue, even after going gluten-free. It can linger for months as the body heals.
- Type 1 Diabetes: 88% experience fatigue, often tied to blood sugar swings and inflammation.
What Actually Helps - Evidence-Based Strategies
There’s no magic pill, but there are proven ways to reduce fatigue. The key is combining approaches. A 2021 Cleveland Clinic study of 1,247 patients found that the most effective strategy was a three-part plan: medication optimization, cognitive behavioral therapy for fatigue, and personalized activity pacing.1. Medication: Targeting the Root
If your HPA axis is suppressed, low-dose hydrocortisone (10-20 mg daily) can help. In trials, it improved fatigue scores by 35-40% in patients with confirmed cortisol deficiency. But it’s not for everyone - only those with documented adrenal dysfunction. For MS-related fatigue, modafinil (a wakefulness agent) reduced fatigue by 28% more than placebo. It’s not a stimulant like caffeine - it works on brain pathways involved in alertness. Newer options are emerging. Anti-IL-6 drugs (like tocilizumab) showed 38% fatigue reduction in early RA trials. CoQ10 supplements (200 mg/day) improved energy levels by 29% in patients with mitochondrial dysfunction. These aren’t yet standard, but they’re promising.2. Movement: The Right Kind of Exercise
You’ve probably heard “exercise helps.” But in autoimmune fatigue, the wrong kind can make things worse. Graded Exercise Therapy (GET) can help - if done correctly. The trick is pacing. Instead of pushing through fatigue, you learn to stay within your energy limits. A 2021 study found that patients who used pacing techniques had a 78% success rate in reducing fatigue. That means: if you have 10 units of energy today, you plan your day around that. Shower first. Rest. Then do laundry. Don’t try to do it all. Gentle movement - walking, yoga, swimming - helps maintain muscle function and reduces inflammation. But intense workouts or long sessions often trigger crashes. Listen to your body. Rest isn’t failure. It’s part of the treatment.3. Sleep and Circadian Rhythm Fix
Poor sleep doesn’t cause autoimmune fatigue - but it makes it worse. Many patients have disrupted melatonin rhythms. Their bodies don’t know when to sleep or wake up. Fixing this starts with consistency. Go to bed and wake up at the same time every day - even on weekends. Get sunlight within 30 minutes of waking. Avoid screens after 9 PM. Use blackout curtains. If you have sleep apnea or restless leg syndrome, treat them. These are common in autoimmune patients and silently drain your energy. Studies show that fixing sleep patterns alone can reduce fatigue by 22-25%.4. Cognitive Behavioral Therapy for Fatigue (CBT-AF)
This isn’t about “thinking positively.” It’s about rewiring how you relate to fatigue. CBT-AF teaches you to identify unhelpful thoughts (“I’m useless because I can’t do everything”) and replace them with realistic ones (“I’m doing what I can today”). It also helps you build a sustainable routine - pacing, energy accounting, and planning rest breaks. In trials, CBT-AF improved fatigue scores 27% more than standard care. And the gains lasted.What Doesn’t Work - And Why
Many patients try everything: supplements, detoxes, keto diets, IV vitamin drips. Some report short-term relief. But few have strong evidence. - High-dose vitamin D: While low levels are common in autoimmune patients, supplementing beyond normal range doesn’t consistently improve fatigue. - Elimination diets: Unless you have celiac or a confirmed food sensitivity, cutting out entire food groups rarely helps fatigue. - Over-exercising: Pushing through fatigue leads to post-exertional malaise - a crash that can last days. This isn’t discipline. It’s self-sabotage. - Ignoring mental health: Depression and anxiety often coexist with autoimmune fatigue. But treating them with antidepressants alone won’t fix the biological drivers. You need both - medication for inflammation and therapy for coping.





February 2, 2026 AT 15:14
Alec Stewart Stewart
Man, this hit home. I’ve been living with lupus for 12 years and no one gets how exhausting it is to just *exist*. I used to feel guilty for napping after brushing my teeth. Now I know it’s my mitochondria screaming for mercy. 🙏
February 2, 2026 AT 20:33
Demetria Morris
It’s frustrating how doctors still treat this like a mental health issue. I had one tell me to ‘try yoga and positive vibes.’ Meanwhile, my IL-6 levels are through the roof and my brain is literally inflamed. This isn’t a mindset problem-it’s a biological war zone.
February 3, 2026 AT 14:22
Geri Rogers
YESSSSSS this is the most accurate breakdown I’ve ever read 😭✨ I’ve been pushing myself for years trying to ‘beat’ the fatigue-turns out I was just burning out my already broken batteries. CoQ10 + pacing changed my life. 200mg daily, no excuses. Also, sleep hygiene isn’t optional-it’s your lifeline. If you’re scrolling at 11pm, you’re sabotaging yourself. Period. 💪🌙
February 5, 2026 AT 12:03
Caleb Sutton
They’re lying. The whole thing’s a pharmaceutical scam. Fatigue isn’t from cytokines-it’s from 5G, fluoride in the water, and the CDC hiding the truth. They don’t want you to know that sunlight and fasting cure everything. They profit off your weakness.
February 7, 2026 AT 08:21
Jamillah Rodriguez
I read this and just sighed. I’m tired of being tired. But honestly? I don’t even have the energy to try any of this. CBT? Pacing? I can’t even get to the pharmacy. 😴
February 8, 2026 AT 03:23
Susheel Sharma
While the biochemical mechanisms presented are compelling, the article exhibits a concerning reductionism in attributing fatigue solely to cytokine activity and mitochondrial dysfunction. One cannot overlook the epigenetic modulation induced by chronic stress, nor the role of gut microbiota dysbiosis-a factor conspicuously absent from the discourse. The proposed interventions, while superficially pragmatic, lack a systems biology perspective. One must question whether this is medicine-or merely symptom management dressed as science.
February 8, 2026 AT 18:22
Janice Williams
This is dangerously misleading. You’re telling people to take hydrocortisone like it’s vitamin C? And you’re endorsing CBT as if it’s a cure? This is the same pseudoscientific garbage that blames patients for not ‘trying hard enough.’ You’re normalizing pharmaceutical dependency while ignoring the real root: environmental toxins and the decline of natural immunity. Shame on you for giving false hope.
February 10, 2026 AT 15:11
Roshan Gudhe
There’s a quiet dignity in exhaustion that no one talks about. It’s not just the body that’s tired-it’s the soul that’s learned to carry invisible weight. We don’t need more pills or protocols. We need a culture that sees the difference between laziness and depletion. You’re not broken. You’re not failing. You’re just living in a world that refuses to acknowledge the cost of survival. 🌿