You hear stories about people who feel totally fine one month, only to discover a fast-growing tumor by chance, sometimes when it’s already spread. These are the cancers that keep both patients and doctors awake at night—the ones with need-for-speed. What really separates those who beat the clock from those who don’t? It’s all about how quickly we catch these fast-moving threats. Today, cutting-edge technology, clever biomarkers, and smarter screening schedules are quietly saving lives—especially for those already in the fast lane of cancer risk.
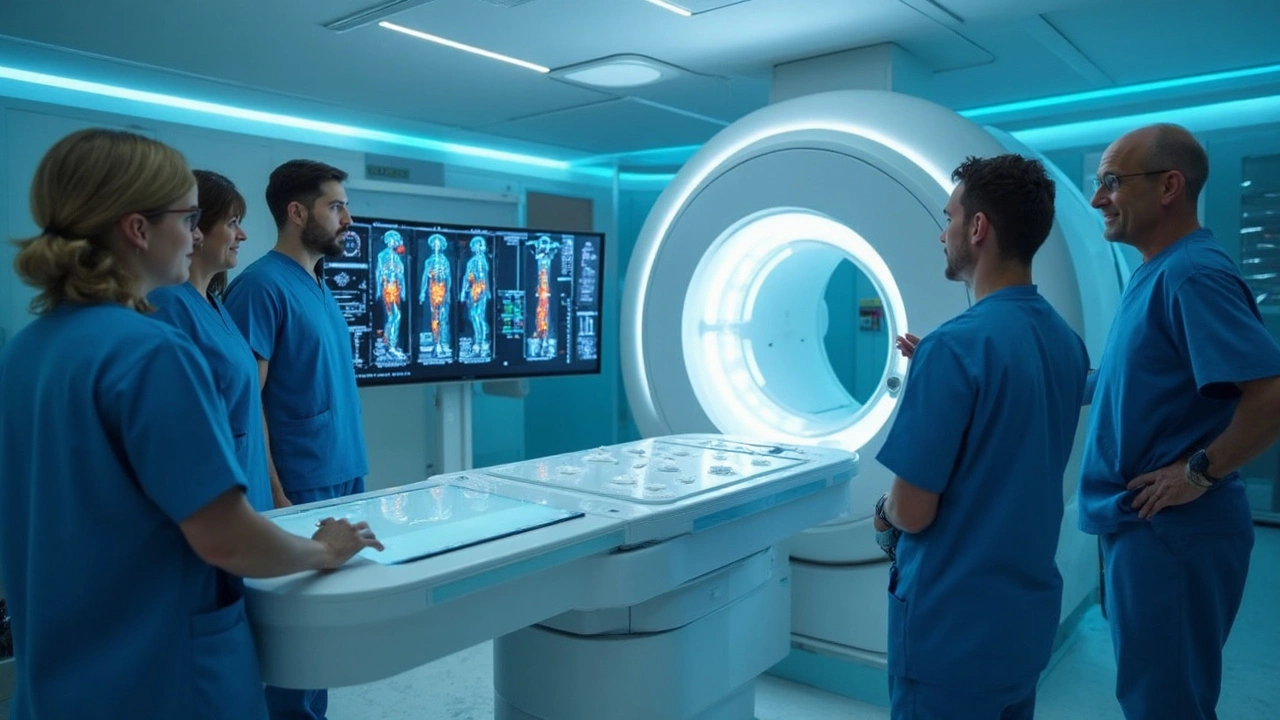
Imaging: Seeing Beyond the Surface
Cancer imaging has come a long way from the blurry X-rays our grandparents remember. Now, doctors wield tools like MRI, CT, PET scans, and even ultrasound machines so precise they’d impress a NASA engineer. These machines are getting better every year at spotting fast-growing tumors early—sometimes before you feel a thing. For example, lung cancer CT scans can see tiny nodules as small as 1-2 millimeters. That’s about the thickness of a penny, and detecting something that small can literally make the difference between life and death.
Fast-growing tumors, like certain types of lung, pancreatic, or aggressive breast cancers, can double in size in just weeks or months. The catch? If your last scan was a year ago, you might miss the window where treatment is simplest and survival odds are highest. That’s why high-risk folks—think smokers, people with strong family cancer histories, or those with rare genetic syndromes—often get put on tighter imaging schedules. For example, some might need scans every three or six months, not just yearly.
But imaging isn’t just about frequency. Advanced MRI with contrast, PET-CT fusion technology, and even new AI-powered algorithms are now flagging hard-to-spot cancers that used to slip under the radar. There’s also the rise of low-dose CT, which cuts down radiation exposure for those who need repeated scans. In 2024, researchers published data showing that lung cancer death rates dropped by 20% in high-risk people who got annual low-dose chest CTs versus chest X-rays. That’s a big leap—and it wouldn’t have been possible without high-resolution imaging.
Imaging is also getting personal. Someone with a BRCA gene mutation, for example, will often have breast MRIs starting in their 20s—much earlier and more often than the average woman. The days of one-size-fits-all screening are fading fast.
Pair this with the new buzz around artificial intelligence. AI isn’t just hype—it can spot patterns in images that the human eye sometimes misses, especially in hard-to-interpret body parts like the pancreas or liver. In a recent clinical setting, AI flagged suspicious spots up to one year before they were visible to doctors. This is wild, but it’s happening right now.
Of course, imaging isn’t perfect. Some fast tumors grow between checks, called "interval cancers." But every step toward sharper, smarter scans pushes the odds back in your favor.
Biomarkers: Cancer Clues in the Blood
Imagine a simple blood test that could warn you about cancer before it takes hold. Sounds like science fiction, but this is quickly turning into our reality. Biomarkers are little chemical flags in the blood, urine, or tissues that hint at the body’s hidden battles—sometimes long before symptoms show up. Tumor DNA, proteins, and even microRNAs leak into circulation as cancers grow, and scientists are learning how to pick up these breadcrumbs.
The classic example is PSA for prostate cancer, but newer tests go way beyond that. One standout star is the "liquid biopsy." Using only a few tubes of blood, these tests can scoop up fragments of tumor DNA that float in your bloodstream. This isn’t just detective work; some liquid biopsies can spot mutations linked to super-fast tumor growth even before a lump is big enough to see on a scan.
This is especially useful for cancers like pancreatic or ovarian, which often skip early warning signs. By tracking shifts in CA19-9 or HE4 levels, doctors can sometimes catch these at an earlier, more curable stage. There’s even progress tracking "circulating tumor cells"—like tiny cancer spies trying to set up shop elsewhere in the body. If you’re at high risk, your doctor might suggest adding a blood biomarker panel to your routine checks, right alongside scans.
Why all the excitement? Data from the last two years shows that combining imaging with biomarkers can bump up early detection rates. Studies from Johns Hopkins and leading European centers found that adding a multi-cancer blood test to standard imaging in high-risk groups caught up to 60% more fast-growing tumors at early, treatable stages.
Still, every test has limits. Some rare cancers don’t leak useful biomarkers, or the signals can get drowned out by non-cancer conditions. That’s why most doctors aren’t tossing out imaging yet. But the days of the blood test "lie detector" for cancer detection are coming closer every month.

Screening Schedules: Timing the Attack
Scheduling isn’t just a logistical headache for cancer clinics; it’s a core part of catching fast tumors. When you know how quickly a cancer type can grow—from a speck to a life-threatening lump—you can plan exactly when to strike. For an up-to-date look at tumor growth speed, check out this deep dive explaining which cancers sprint and which ones crawl.
High-risk patients rarely get the cookie-cutter treatment. If you’ve got a genetic cancer syndrome—say, Lynch or Li-Fraumeni syndrome—your actual risk of cancer may be dozens of times higher than the average person. Those folks go on tailored screening plans, sometimes starting in their teens or twenties. The intervals often shrink to months instead of years, especially for cancers that double quickly. For example, someone at high risk for hepatocellular carcinoma (liver cancer) might get an ultrasound and blood test every six months, year after year.
Table: Examples of Cancer Screening Schedules for High-Risk Patients
| Cancer Type | Standard Population | High-Risk Patients |
|---|---|---|
| Breast (BRCA+) | Mammogram every 1-2 years, age 40+ | MRI AND mammogram yearly, age 25+ |
| Colon (Lynch syndrome) | Colonoscopy every 10 years, age 45+ | Colonoscopy every 1-2 years, age 20-25+ |
| Liver (HBV, cirrhosis) | No routine screening | Ultrasound & AFP blood test every 6 months |
| Pancreas (family history) | No routine screening | MRI and/or endoscopic ultrasound every 1 year, age 50+ |
Some of these plans might seem intense or even scary, but catching a nodule at 2mm instead of 5cm is game-changing. That extra time can mean fewer surgeries, more treatment options, and way higher odds of making it to remission. Patients who stick to their screening plans (and speak up if they notice new symptoms in between) consistently catch more tumors early, according to tracking from major cancer registries.
Of course, with frequent screening comes the risk of false alarms. Not every shadow or bump is cancer. This is why top centers now use risk calculators—factoring in genetics, lifestyle, age, and even prior scan data—to decide when and how to test. It helps keep the focus on those most likely to benefit, without overwhelming folks with unnecessary worry.
Want a tip? If cancer runs in your family or you know you’re at high risk, talk to your doctor about a personalized schedule, not the default one. The evidence is clear: catching fast growers means thinking ahead, not just reacting.
Tips for High-Risk Patients and Future Directions
So, what can you actually do if you’re one of the millions in a cancer “high-alert” category? First, stay on top of your screening appointments. Sounds simple, but skipping scans by even a few months can mean the difference between curable and not. Second, ask whether you qualify for newer blood-based tests—liquid biopsies are rolling out at more clinics every year, and they take just a few minutes for a blood draw.
If your family has a gnarly cancer history, genetic testing might reveal if you should be on an aggressive screening plan. Several insurance companies now cover this for folks with certain risk profiles. Don’t be shy to bring it up. Frequent skin checks, self-breast exams, or learning the subtle warning signs for pancreatic or ovarian cancer (unexpected weight loss, odd stomach pain) can tip you off sooner. Smartwatches, believe it or not, have helped catch tumors early by flagging unexpected heart rhythm changes, although that’s still rare. But hey, tech is moving fast everywhere.
For those who want to know about the science of catching fast tumors, keep your eyes peeled for advances in artificial intelligence. AI is set to turbocharge everything—making scans sharper, blood tests smarter, and even predicting personal risk down to the week. Researchers in the past year launched pilot trials using AI to look at regular scan sequences over time, spotting fast changes even before symptoms show up. The hope? Instead of catching up to cancer, we’ll soon be outpacing it entirely.
How about cost? While some new tests are pricey, many imaging and screening strategies are covered by national health plans for high-risk groups. Technology is getting cheaper, too. Liquid biopsy kits that cost thousands five years ago are now being bundled into routine checkups in major hospitals. This democratization might be the great game-changer.
More is coming. In 2025, researchers are studying combo-screening—pairing ultra-low-dose CT, two blood markers, and AI analysis, looking for those rogue tumors that otherwise hide. Early trial data from Japan and the US suggests this combo can flag up to 70% of dangerous cancers before symptoms crash the party. That’s not perfect, but it’s the lifeline many need.
So, if you ever feel like you’re racing against the clock, you probably are. But with early tumor detection in your corner—using top-shelf imaging, clever biomarkers, and personalized screening schedules—you’ve got a real shot of spotting fast-growing tumors before they can do serious damage. Stay curious, talk to your health team, and bet on the science: the odds keep improving every year.




May 26, 2025 AT 16:31
Anthony Griek
Had a cousin go through this last year. They caught her breast cancer early because she insisted on the MRI despite her doctor saying yearly mammogram was fine. Turned out she had a BRCA mutation. Now she’s in remission. Just goes to show-don’t take ‘standard’ as gospel if your family history screams otherwise.
May 28, 2025 AT 15:56
Norman Rexford
man i swear america’s healthcare system is the only one that makes you wait until you’re practically dead before they check for cancer. i mean cmon we got drones that deliver pizza but you gotta beg for a ct scan if you’re not rich? 🤡
May 29, 2025 AT 12:47
Wayne Keller
Really appreciate how this breaks it down. A lot of people don’t realize that screening isn’t one-size-fits-all. If you’ve got a family history, pushing for earlier or more frequent tests isn’t being dramatic-it’s smart. And yeah, liquid biopsies are getting real. My uncle got one last year after a weird AFP spike. Turned out nothing, but at least we knew.
May 31, 2025 AT 11:33
Shana Labed
OMG I JUST FOUND OUT MY MOM HAS LYNCH SYNDROME AND I’M GETTING A COLONOSCOPY NEXT WEEK 😭 I WAS SO SCARED BUT NOW I’M LIKE… THIS IS MY SUPERPOWER. I’M BEATING THE CLOCK BEFORE IT EVEN STARTS. 🙌🩺 #earlydetectionislife
June 1, 2025 AT 18:56
California Daughter
Wait… so you’re telling me we’re not all just supposed to get a full-body MRI every year… just in case? Like… why isn’t this standard? Are we really still relying on ‘if you feel something, come back’? That’s not medicine, that’s Russian roulette with your organs.
June 2, 2025 AT 14:58
Vishwajeet Gade
usa spending billions on ai cancer scans but in india we still use 1990s machines. why? because rich people get care. poor people get luck. its sad. my dad died from liver cancer because no one checked him until it was too late. no one even asked if he had hbv.
June 2, 2025 AT 21:58
Casey Crowell
Just got my first liquid biopsy results back-negative. But honestly? I’m not relieved because I’m lucky. I’m relieved because science is finally catching up. 🤖💉 This isn’t sci-fi anymore. It’s Tuesday. And if you’re high-risk and not asking your doc about this, you’re doing yourself a disservice. #TechIsWinning
June 3, 2025 AT 16:45
Shanna Talley
If you’re reading this and you’ve got a family history-do something. Not tomorrow. Not next year. Now. One scan, one blood test, one conversation with your doctor can change everything. You don’t need to be a hero. Just be consistent. The science is already there. You just have to show up.