Dose Titration Timeline Calculator
See how slow dose increases reduce side effects. Select your medication type to view the typical titration schedule and side effect risks.
Titration Timeline
Side Effect Reduction:
Following this titration schedule can reduce initial side effects by 40-60% compared to starting at full dose.
Patient Tips
- Track symptoms daily using a 1-10 scale Recommended
- Wait 1-2 weeks between dose increases Critical
- Report side effects to your doctor immediately Essential
- Don't skip appointments during titration Important
Why Dose Titration Matters for Your Medication Safety
Imagine starting a new medication and feeling dizzy, nauseous, or anxious within days-so bad you quit taking it. This happens more often than you think. But what if you could avoid those side effects altogether? The answer isn’t stopping the drug-it’s dose titration. This isn’t just a medical buzzword. It’s a proven, step-by-step method used by doctors to find the lowest effective dose that works for you, without wrecking your day.
According to the American Medical Association, 87% of prescription drugs with serious side effects now come with official titration guidelines. That’s because many medications-like those for ADHD, depression, epilepsy, or heart failure-have a narrow window between helping you and hurting you. Too much too fast? Side effects spike. Too little? You get no benefit. Titration walks that line carefully, so you don’t have to guess.
How Dose Titration Actually Works
Dose titration means starting low and going slow. Instead of jumping to the full prescribed dose, your doctor begins with a fraction-often 25% to 50%-and increases it gradually. The goal? Let your body adjust before adding more pressure.
For stimulant medications like Adderall or Vyvanse used in ADHD, the typical schedule is a 10% to 25% increase every 3 to 7 days. For slower-acting drugs like atomoxetine or certain antidepressants, you might wait 1 to 2 weeks between adjustments. Some medications need even longer: lamotrigine for epilepsy can take up to 5 weeks just to reach a moderate dose, because going too fast can trigger a dangerous skin reaction called Stevens-Johnson syndrome.
Take venetoclax, a cancer drug. Its titration schedule is strict: 20 mg in week one, then 50 mg, 100 mg, 200 mg, and finally 400 mg by week five. This isn’t arbitrary. It’s designed to prevent tumor lysis syndrome-a life-threatening condition that happens when cancer cells die too quickly. Without this slow ramp-up, the risk jumps dramatically.
Real Side Effects You Can Avoid With Titration
Studies show titration can cut initial side effects by 40% to 60%. Here’s what that looks like in real life:
- Starting Adderall at 5 mg instead of 10 mg reduces anxiety, insomnia, and appetite loss by half.
- Slowly increasing levothyroxine for hypothyroidism prevents heart palpitations and bone loss that happen with sudden dose jumps.
- Gradual up-titration of beta-blockers in heart failure patients cuts dropout rates due to fatigue or dizziness from 45% down to 18%, according to the American Heart Association.
A 2022 survey of 1,200 ADHD patients found that 74% who followed a proper titration plan reported side effects they could manage. Only 41% of those who skipped titration said the same. One Reddit user wrote: “Starting at 5 mg Adderall instead of 10 mg saved me from horrible anxiety. I stayed on it for 3 years.” Another said: “My doctor started me at full dose. I quit for two years because I felt like I was losing my mind.”
Which Medications Need Titration the Most?
Not all drugs need this careful approach. But these do:
- ADHD medications: Stimulants (Adderall, Ritalin, Vyvanse) and non-stimulants (Strattera, Intuniv) both require titration. Up to 78% of ADHD patients need at least one dose adjustment in the first few months.
- Antidepressants: SSRIs like sertraline or fluoxetine often cause nausea, agitation, or sleep issues early on. Starting low reduces dropout rates.
- Anticonvulsants: Lamotrigine, perampanel, and valproate all carry risks of severe rashes or liver issues if dosed too quickly.
- Heart and blood pressure drugs: Beta-blockers (metoprolol, carvedilol), ACE inhibitors, and diuretics need slow increases to avoid low blood pressure or kidney stress.
- Anticoagulants: Warfarin requires weekly blood tests (INR) and tiny adjustments. Newer drugs like apixaban are more forgiving-but even they benefit from cautious starts.
- Cancer drugs: Venetoclax, ibrutinib, and others have strict titration schedules built into their FDA labels.
Compare warfarin to apixaban: 67% of warfarin patients need dose changes in the first month. Only 28% of apixaban users do. That’s because warfarin’s therapeutic range is razor-thin-too little and you clot; too much and you bleed. Titration isn’t optional here. It’s survival.
What You Can Do to Make Titration Work for You
Titration isn’t just your doctor’s job. Your input matters.
- Track symptoms daily. Use a simple 1-to-10 scale: rate side effects like dizziness, sleep, appetite, mood, and energy. Write them down. A 2023 Healthgrades survey found that 78% of patients who kept a side effect journal had better outcomes.
- Take meds at the same time every day. Even a 30-minute shift can throw off how your body responds. Consistency helps your doctor spot real trends.
- Don’t skip appointments. Weekly check-ins during titration aren’t optional. Missing one can mean a wrong dose adjustment.
- Ask about food interactions. Some drugs (like lamotrigine or venetoclax) are better tolerated when taken with food. Others need an empty stomach. Ask your pharmacist.
- Speak up early. If you feel worse after a dose increase, call your doctor before the next visit. Don’t wait. You might need to hold the dose or even go back a step.
One common mistake? Mistaking side effects for normal stress. A 2021 BMC Psychiatry study found that 58% of patients couldn’t tell if their fatigue or irritability came from the drug or life. That’s why waiting 1 to 2 weeks between dose changes is critical-it gives your body time to stabilize.
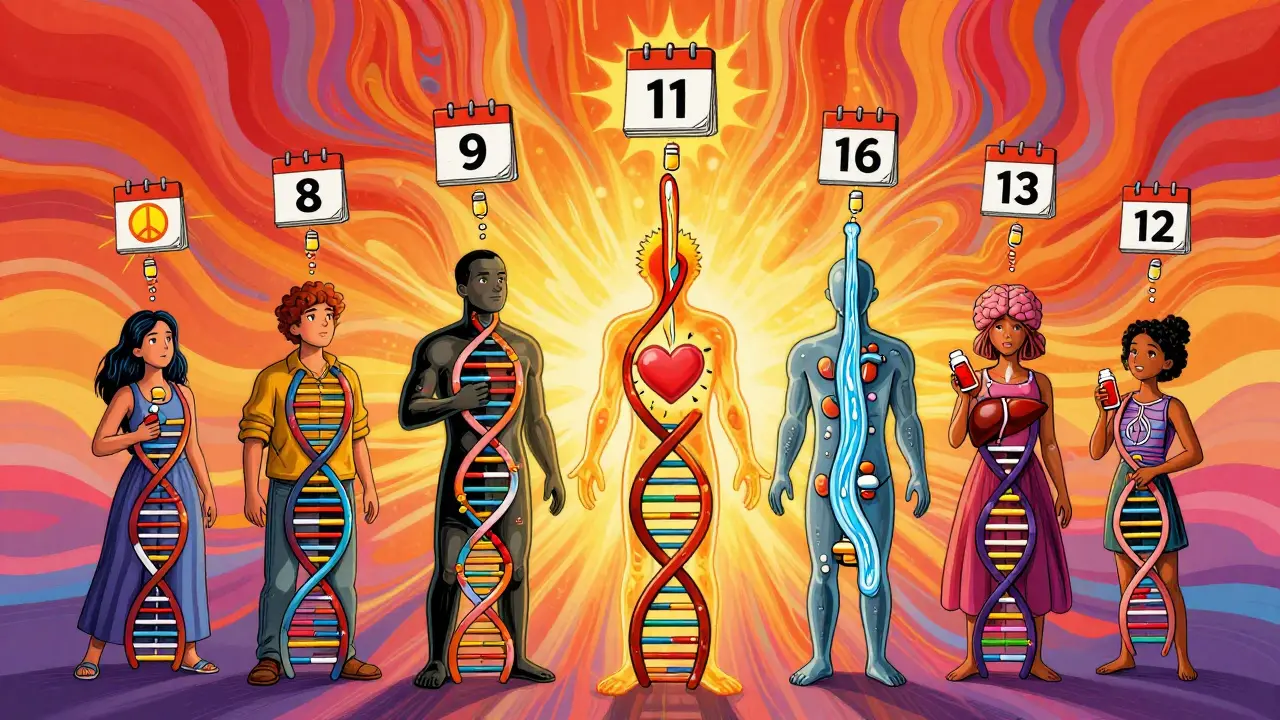
The New Tools Making Titration Easier
Titration isn’t stuck in the past. Technology is helping.
In January 2023, the FDA cleared the first AI-powered app for dose titration: TitrationTracker. It asks you to log your symptoms weekly, then uses algorithms to suggest the best next dose. A 2023 study in Nature Digital Medicine showed it reduced side effects by 32% compared to standard care.
Even better? Pharmacogenetic testing is starting to guide starting doses. For 28 medications-including antidepressants, painkillers, and statins-your genes can tell your doctor if you’re a fast or slow metabolizer. That means your first dose might be lower or higher based on your DNA. By 2025, 12 more drugs will get this kind of guidance. By 2030, experts predict 75% of high-risk medications will use genetic titration as standard.
Meanwhile, the global market for therapeutic drug monitoring-blood tests that guide dosing-is projected to hit $4.1 billion by 2027. That’s because doctors are finally catching on: precision dosing saves money, reduces hospital visits, and keeps people on their meds.
When Titration Isn’t the Answer
Titration isn’t magic. It has limits.
In emergencies-like a heart attack, seizure, or allergic reaction-you need fast action. There’s no time to wait weeks for a dose to build up. In those cases, immediate high doses are necessary.
Also, if you’re severely depressed or suicidal, waiting 8 weeks to feel better isn’t safe. Some psychiatrists will start higher doses faster in these cases, balancing risk and urgency. As Dr. Alan F. Schatzberg from Stanford warned: “Overly conservative titration can lead to undertreatment.”
And in places with limited healthcare access-like rural areas or low-income countries-weekly visits aren’t possible. The WHO reports only 22% of low-income nations have formal titration protocols for essential drugs. That’s a gap we still need to fix.
What to Expect During Your Titration Journey
Most titration plans last 4 to 12 weeks. You’ll need to commit:
- 15 to 20 minutes a day to track symptoms.
- Weekly check-ins with your provider.
- Patience. You might not feel better for weeks-even as the dose climbs.
But the payoff is real. You’re not just avoiding side effects. You’re finding the dose that lets you live your life-not fight your medication.
And here’s the kicker: once you find your sweet spot, you’ll likely stay there for years. That’s the goal. Not to be on the highest dose possible. But to be on the right dose for you.
What is the purpose of dose titration?
The purpose of dose titration is to find the lowest effective dose of a medication that controls symptoms while minimizing side effects. This is especially important for drugs with a narrow therapeutic index, where the difference between a helpful dose and a harmful one is small. By starting low and increasing slowly, your body adjusts, reducing the risk of severe reactions and improving long-term adherence.
How long does dose titration usually take?
It varies by medication. For stimulants like Adderall, titration often takes 4 to 6 weeks. For non-stimulants like Strattera or antidepressants, it can take 8 to 12 weeks. Some drugs, like lamotrigine or venetoclax, require even longer schedules-up to 5 or more weeks-to prevent life-threatening side effects. The timeline is always based on how quickly the drug works in your body and how sensitive you are to its effects.
Can I adjust my dose myself if I feel side effects?
No. Never change your dose without talking to your doctor. Even small changes can cause serious problems. For example, suddenly stopping an antidepressant can trigger withdrawal symptoms. Raising a dose too fast can cause seizures, heart issues, or toxic reactions. Titration is a medical process that requires monitoring. If side effects are severe, contact your provider immediately-they may pause the increase or lower the dose temporarily.
Why do some doctors skip titration and start at full dose?
Sometimes, it’s due to time pressure, lack of awareness, or misjudging patient risk. In cases of severe illness-like major depression or uncontrolled seizures-some providers opt for faster dosing to get results quickly. But this approach increases side effect risks and dropout rates. The standard of care now strongly favors titration, especially for ADHD, psychiatric, and cardiac drugs. If your doctor skips it, ask why-and if they can follow a slower, safer plan.
Are there digital tools to help with titration?
Yes. The FDA-cleared TitrationTracker app, launched in January 2023, uses AI to analyze your daily symptom logs and suggest optimal dose changes. Research shows it reduces side effects by 32% compared to traditional methods. Other tools include digital pill trackers, EHR-integrated dosing calculators, and wearable sensors that monitor heart rate or sleep patterns. These tools make titration more precise and less burdensome for patients and providers.
Does genetic testing play a role in titration?
Yes, and it’s growing fast. For 28 medications-including certain antidepressants, painkillers, and cholesterol drugs-genetic tests can tell if you’re a fast or slow metabolizer. This helps doctors choose your starting dose. For example, if you metabolize a drug slowly, you might start at half the usual dose to avoid buildup and side effects. By 2025, 12 more drugs will have official genetic dosing guidelines. Experts predict this will become standard for 75% of high-risk medications by 2030.
Next Steps: What to Do Today
If you’re starting a new medication with known side effects, ask your doctor: “What’s the titration plan?” Don’t assume it’s built in. If they say “just take one pill a day,” push back. Request the official schedule from the drug manufacturer-it’s often available online.
Download a free symptom tracker app or print a simple chart. Start logging your mood, sleep, appetite, and energy level daily. Bring it to every appointment. If you’ve been on a drug for months and still feel awful, it might not be your condition-it might be your dose. Ask about titration again. You deserve to feel better, not just medicated.






January 26, 2026 AT 18:14
Henry Jenkins
I've been on Vyvanse for 5 years and this is the first time I've seen someone break down titration like this. Starting at 10mg was a nightmare-panic attacks, insomnia, lost 15lbs in two weeks. Went back to my doc, they agreed to restart at 5mg and bump 2.5mg every 10 days. Took 8 weeks but now I'm stable, focused, and actually sleeping. This isn't just medical advice-it's survival. Why do so many docs treat this like a one-size-fits-all script?
Also, the AI tracker thing? I tried a free app called MedTrack. It synced with my Apple Health and flagged when my heart rate spiked after dose changes. Saved me from a hospital trip. Maybe not FDA-cleared, but it works.
January 27, 2026 AT 16:53
Dan Nichols
Titration my ass. I got prescribed 20mg of sertraline and took it day one. Felt like a zombie for 3 days then it kicked in. No drama. No journaling. No apps. Just took the damn pill. Now I'm fine. All this overcautiousness is just fearmongering by Big Pharma to sell more visits and apps. If your body can't handle a standard dose you're not the right candidate for the drug. Stop infantilizing patients.
January 28, 2026 AT 07:58
Renia Pyles
I started lamotrigine at full dose because my psychiatrist was in a hurry. I got Stevens-Johnson. Spent 17 days in the ICU. My skin peeled off in sheets. I still have scars. They told me it was 'rare'. It wasn't rare. It was predictable. And now they want me to trust their 'titration schedules'? I don't trust any doctor who doesn't treat me like a human with a nervous system. This isn't science-it's gambling with your body.
January 29, 2026 AT 02:45
Rakesh Kakkad
In India, we do not have access to such sophisticated titration protocols. Many patients receive full doses due to lack of follow-up infrastructure. The WHO report cited is accurate. However, in rural areas, even basic blood pressure monitoring is a luxury. We need systemic change, not apps. Digital tools help the privileged, but for the 80% without smartphones or clinics, the solution is community health workers trained in basic titration principles. Technology without equity is just another form of exclusion.
January 29, 2026 AT 16:47
Nicholas Miter
I was skeptical about titration too until I started on metoprolol for hypertension. Went from 25mg to 50mg in 4 days and felt like I was drowning. My legs were heavy, my head foggy. Called my nurse, she told me to drop back to 25mg and wait two weeks. Did it. Now I'm at 50mg and feel great. The key is patience. And honestly? Tracking symptoms isn't that hard. I just use the notes app on my phone. One line a day. 'Sleep: 5/10. Dizzy after lunch.' That's it. No fancy apps needed.
January 30, 2026 AT 16:11
Suresh Kumar Govindan
The FDA-approved AI tracker is a distraction. The real issue is that 90% of prescribers are not trained in pharmacokinetics. Titration is not a protocol-it's a skill. And most doctors are rushed, overworked, and incentivized to move patients through quickly. The app doesn't fix the system. It masks it. Meanwhile, genetic testing? Only available to the wealthy. This is precision medicine for the elite. The rest of us get lucky guesses.
February 1, 2026 AT 06:15
George Rahn
America has turned medication into a cult. We worship the pill, then panic when it hurts. Titration isn't about safety-it's about control. The system wants you dependent, doc-dependent, app-dependent. But here's the truth: your body is smarter than your doctor's algorithm. I took my first dose of Prozac at full strength. Felt weird. Didn't like it. Stopped. Two weeks later, I felt better than I had in years. No titration. No journal. Just listening. Sometimes the most radical act is saying no.
February 2, 2026 AT 19:47
Ashley Karanja
I just want to say how deeply this resonates. As someone with treatment-resistant depression, I’ve cycled through 7 different SSRIs. Each time, I was thrown into the deep end. The first time I was given a titration plan? I cried. Not because I was happy-because for the first time, someone treated me like I was worth the time. I tracked my mood on a paper calendar. Drew little suns and clouds. My therapist said it looked like a weather map of my soul. It took 10 weeks to find the right dose of escitalopram. I still use the calendar. It’s my reminder that healing isn’t linear, and that slow is sacred. 🌱
February 3, 2026 AT 04:13
Karen Droege
I’m a nurse and I’ve seen this play out a hundred times. A patient starts a new med, panics after 3 days, quits, and then blames the drug. Meanwhile, the doctor never explained titration. Not because they’re lazy-but because they assume the patient knows. They don’t. We need a standardized patient handout-like the ones for chemo or insulin-explaining what to expect week by week. And we need to stop acting like side effects are a personal failure. They’re a biological response. The system needs to meet people where they are. Not the other way around.