Folate Deficiency: What It Is, Why It Matters, and How to Fix It
When dealing with folate deficiency, a condition where the body lacks adequate folate (vitamin B9) for normal cellular function. Also known as low folate, it can lead to serious health issues if left unchecked.
Key Aspects of Folate Deficiency
The most direct driver of folate deficiency is insufficient folic acid, the synthetic form of folate found in supplements and fortified foods. Folic acid is essential for DNA synthesis, red‑blood‑cell formation, and proper brain development. When intake drops, the body can’t keep up with rapid cell turnover, so the condition encompasses low blood folate levels.
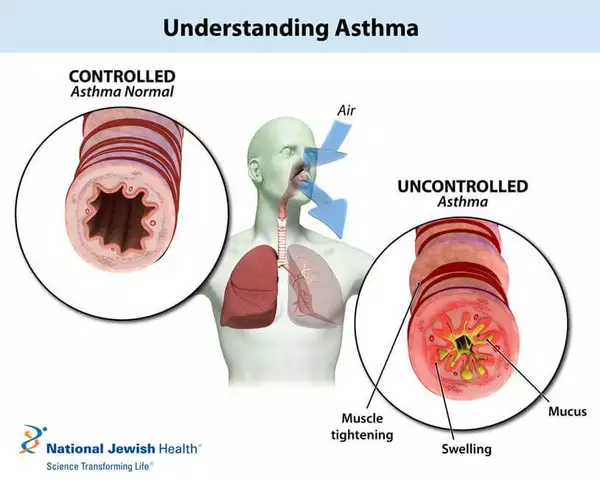
One of the first clinical signs of anemia, specifically megaloblastic anemia, is a direct result of folate deficiency. The shortage of folic acid hampers red‑cell maturation, leading to larger, less functional cells. In plain terms, folate deficiency requires adequate folic acid to prevent this type of anemia.
Pregnant women are especially vulnerable. During early pregnancy, a mother's folate stores support the developing neural tube, which becomes the brain and spinal cord. When folate deficiency influences the fetus, the risk of neural tube defects like spina bifida spikes dramatically. That’s why prenatal vitamins always spotlight folic acid.
Neural tube defects themselves are a clear illustration of how folate deficiency affects fetal development. Even a modest shortfall can impair the closure of the neural tube within the first month of conception, leading to lifelong disability. This connection makes folate screening a routine part of pre‑conception care.
Beyond folic acid, other nutrients interact with folate metabolism. Vitamin B12, for instance, works hand‑in‑hand with folate to produce healthy red blood cells. A deficiency in B12 can masquerade as folate deficiency, confusing diagnosis. Knowing this relationship helps clinicians choose the right lab tests.
Testing is straightforward: a simple blood test measures serum folate and red‑cell folate levels. If results show low values, doctors will often ask about diet, medication use, and any malabsorption issues like celiac disease. This diagnostic step enables targeted treatment.
Treatment usually starts with diet changes—leafy greens, beans, citrus fruits, and fortified grains are top sources of natural folate. If diet alone isn’t enough, a daily supplement of 400–800 µg of folic acid is standard for most adults, while pregnant women may need up to 1 mg. Proper dosing ensures blood folate levels return to normal, reducing anemia risk and protecting future pregnancies.
Now that you’ve got a clear picture of what folate deficiency looks like, why it matters, and how to address it, the articles below dive deeper into related medications, supplement options, and lifestyle tips. Browse the collection to find detailed guides on managing low folate, choosing the right supplement, and understanding how other drugs may interact with your treatment plan.
Folate Deficiency and Hormone Imbalances: How Low Folate Affects Your Hormones
Explore how folate deficiency disrupts hormone balance, who’s at risk, how to test, and practical diet and supplement steps to restore healthy estrogen, testosterone, thyroid and cortisol levels.